What Is Considered The Functional Unit Of The Kidney
News Leon
Mar 26, 2025 · 6 min read
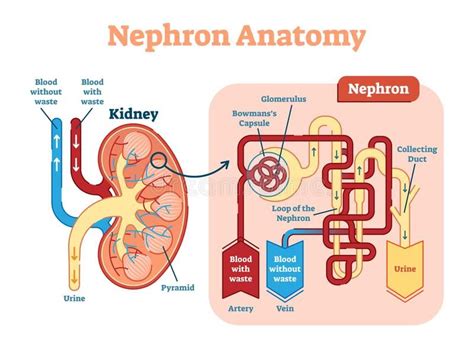
Table of Contents
What is Considered the Functional Unit of the Kidney?
The kidney, a vital organ in the human body, plays a crucial role in maintaining overall health and well-being. Its primary function is to filter blood and remove waste products, excess water, and other impurities to produce urine. But what exactly is the fundamental unit responsible for carrying out these complex processes within the kidney? The answer is the nephron. This article will delve deep into the structure and function of the nephron, explaining why it's rightfully considered the functional unit of the kidney. We'll explore its intricate components, the processes involved in urine formation, and the implications of nephron dysfunction.
Understanding the Nephron: The Workhorse of the Kidney
The nephron is the microscopic structural and functional unit of the kidney. Each kidney contains approximately one million nephrons, and their combined efforts are responsible for the kidney's overall function. These tiny, complex structures are responsible for filtering blood, reabsorbing essential nutrients, and excreting waste products. The efficiency and number of functioning nephrons directly impact the kidney's ability to perform its vital tasks.
The Key Components of a Nephron
A nephron consists of two main parts:
1. The Renal Corpuscle (Malpighian Body): This is the initial filtering unit of the nephron. It comprises two structures:
-
Glomerulus: A network of capillaries where blood filtration begins. The glomerulus is surrounded by a specialized structure called Bowman's capsule. The high pressure within the glomerular capillaries forces fluid and small molecules out of the blood and into Bowman's capsule. This process is called glomerular filtration. The glomerular filtration rate (GFR) is a crucial indicator of kidney function. A decreased GFR suggests impaired kidney function.
-
Bowman's Capsule (Glomerular Capsule): A double-walled cup-shaped structure surrounding the glomerulus. It collects the filtrate produced during glomerular filtration. This filtrate, while initially similar to plasma, lacks large proteins and blood cells.
2. The Renal Tubule: This long, convoluted tube extends from Bowman's capsule and plays a critical role in modifying the filtrate. It's divided into several segments:
-
Proximal Convoluted Tubule (PCT): The first segment of the renal tubule. It's responsible for the majority of reabsorption of essential substances like glucose, amino acids, water, sodium, and bicarbonate ions back into the bloodstream. This process is vital for preventing the loss of valuable nutrients and maintaining the body's electrolyte balance. The PCT also actively secretes substances like hydrogen ions and drugs.
-
Loop of Henle: This U-shaped structure extends from the PCT deep into the renal medulla. The loop of Henle plays a crucial role in concentrating the urine by establishing a concentration gradient in the medulla. The descending limb is highly permeable to water, while the ascending limb is impermeable to water but actively transports sodium, chloride, and potassium ions out of the tubule. This countercurrent multiplier system is essential for conserving water.
-
Distal Convoluted Tubule (DCT): The final segment of the renal tubule before the collecting duct. The DCT plays a crucial role in fine-tuning the composition of the filtrate by regulating the reabsorption of sodium, potassium, calcium, and other ions. It also contributes to acid-base balance through the secretion of hydrogen ions. The action of aldosterone, a hormone released by the adrenal glands, strongly influences sodium and potassium reabsorption in the DCT.
-
Collecting Duct: This is not technically part of the nephron, but it receives filtrate from multiple nephrons and plays a crucial role in final urine concentration. The collecting ducts are highly permeable to water under the influence of antidiuretic hormone (ADH), which is produced by the hypothalamus and stored in the posterior pituitary gland. ADH regulates water reabsorption, helping the body conserve water when needed.
The Processes of Urine Formation: A Detailed Look
Urine formation involves three main processes:
1. Glomerular Filtration: This is a passive process driven by the hydrostatic pressure difference between the glomerular capillaries and Bowman's capsule. Water and small dissolved substances are forced through the filtration membrane, which is composed of the fenestrated capillaries, the glomerular basement membrane, and the podocytes of Bowman's capsule. Larger molecules like proteins and blood cells are generally excluded from the filtrate.
2. Tubular Reabsorption: This is an active and passive process where essential nutrients, water, and ions are reabsorbed from the filtrate back into the bloodstream. The majority of reabsorption occurs in the proximal convoluted tubule, while the loop of Henle and distal convoluted tubule fine-tune the process. The reabsorption mechanisms involve various transport proteins and channels located on the epithelial cells lining the renal tubules. This ensures that valuable substances are not lost in the urine.
3. Tubular Secretion: This is an active process where substances are transported from the peritubular capillaries (the blood vessels surrounding the renal tubules) into the renal tubules. This process helps to eliminate waste products and regulate the pH of the blood. Examples of substances secreted include hydrogen ions, potassium ions, and certain drugs. Tubular secretion further contributes to the fine-tuning of the urine composition.
The Importance of Nephron Function in Overall Health
The proper function of nephrons is essential for maintaining homeostasis—the body's internal balance. Nephrons work tirelessly to:
- Regulate blood pressure: By adjusting the volume of water and electrolytes in the body.
- Maintain electrolyte balance: Ensuring the appropriate levels of sodium, potassium, calcium, and other ions.
- Excrete waste products: Removing metabolic byproducts like urea, creatinine, and uric acid.
- Regulate blood pH: By excreting hydrogen ions or bicarbonate ions.
- Produce erythropoietin: A hormone that stimulates red blood cell production.
- Activate Vitamin D: A crucial vitamin for calcium absorption.
Nephron Dysfunction and Kidney Disease
Damage or dysfunction of nephrons can lead to various kidney diseases. Several factors can contribute to nephron damage, including:
- Diabetes: High blood sugar levels can damage the glomeruli and other parts of the nephrons.
- High blood pressure: Can damage the blood vessels supplying the kidneys.
- Autoimmune diseases: Conditions like lupus and glomerulonephritis can cause inflammation and damage to the nephrons.
- Genetic disorders: Certain inherited conditions can affect the development or function of nephrons.
- Kidney infections: Infections can cause inflammation and scarring of the nephrons.
- Obstruction: Blockages in the urinary tract can lead to back pressure and nephron damage.
The progressive loss of nephrons leads to chronic kidney disease (CKD), a serious condition that can eventually lead to kidney failure requiring dialysis or kidney transplantation. Early detection and management of risk factors are crucial for preventing or slowing the progression of kidney disease.
Clinical Significance and Diagnostic Tests
Assessing nephron function is crucial in diagnosing and managing kidney diseases. Several tests are commonly used to evaluate kidney function, including:
- Glomerular filtration rate (GFR): A measure of how well the kidneys are filtering blood.
- Blood urea nitrogen (BUN) and creatinine levels: Indicators of waste product accumulation in the blood.
- Urine analysis: Examines the composition of the urine to detect abnormalities.
- Kidney biopsy: A procedure where a small sample of kidney tissue is removed for microscopic examination.
Conclusion: The Unsung Hero of Renal Physiology
The nephron, as the functional unit of the kidney, plays a multifaceted role in maintaining overall health. Its intricate structure and complex functions are essential for blood filtration, waste excretion, and electrolyte balance. Understanding the nephron's structure and processes is fundamental to appreciating the kidney's critical role in homeostasis. The consequences of nephron dysfunction underscore the importance of maintaining healthy kidney function through lifestyle choices and early detection of kidney disease. The ongoing research into nephron physiology and the development of new therapeutic strategies continue to improve our understanding and treatment of kidney diseases, improving the quality of life for millions. The nephron, though microscopic, is a true unsung hero of renal physiology, ensuring our bodies function optimally.
Latest Posts
Latest Posts
-
What Is The Stationary Phase For Paper Chromatography One Word Answer
Mar 29, 2025
-
Part Of Line With Two Endpoints
Mar 29, 2025
-
What Is The Density Of Cork In G Cm3
Mar 29, 2025
-
The Capacity Of A Communication Channel Is Measured In
Mar 29, 2025
-
Are Frogs Omnivores Carnivores Or Herbivores
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about What Is Considered The Functional Unit Of The Kidney . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
