The Basic Difference Between Spermatogenesis And Oogenesis Is That
News Leon
Mar 23, 2025 · 7 min read
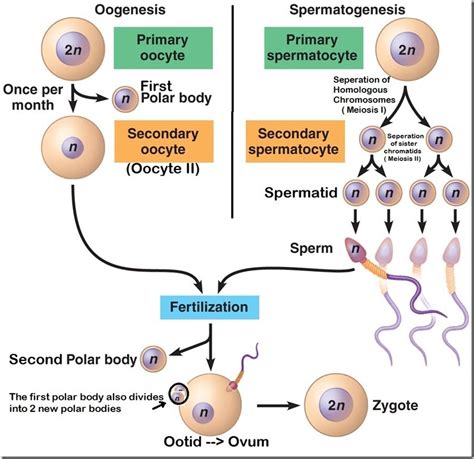
Table of Contents
The Basic Difference Between Spermatogenesis and Oogenesis: A Comprehensive Overview
Spermatogenesis and oogenesis are fundamental processes in sexual reproduction, responsible for the production of male and female gametes – sperm and ova, respectively. While both processes share similarities in their underlying mechanisms, such as meiosis, they also exhibit crucial differences that reflect the distinct reproductive roles of males and females. Understanding these differences is key to grasping the complexities of human reproduction and related conditions. This comprehensive article will delve into the core distinctions between spermatogenesis and oogenesis, covering their timelines, locations, products, and regulatory mechanisms.
Key Differences: A Quick Glance
Before diving deep, let's summarize the primary distinctions:
| Feature | Spermatogenesis | Oogenesis |
|---|---|---|
| Location | Seminiferous tubules of the testes | Ovaries |
| Timing | Continuous from puberty to death | Begins prenatally, pauses, and resumes at puberty |
| Product | Four haploid, motile sperm cells per meiosis | One haploid ovum and three polar bodies per meiosis |
| Cytoplasm | Cytoplasm divided equally among sperm cells | Cytoplasm mostly retained by the ovum |
| Size | Small, motile cells | Large, non-motile cell |
| Duration | Relatively short | Relatively long |
| Hormonal Control | Primarily testosterone | Primarily FSH and LH |
Spermatogenesis: The Journey of Sperm Production
Spermatogenesis, the process of sperm production, is a continuous process that begins at puberty and continues throughout a male's lifespan. It occurs within the seminiferous tubules of the testes, intricate structures lined with Sertoli cells and germ cells at various stages of development.
Stages of Spermatogenesis:
-
Spermatocytogenesis: This initial phase involves mitotic divisions of spermatogonial stem cells (diploid). These stem cells undergo self-renewal, maintaining a pool of stem cells for continuous sperm production. One daughter cell remains a stem cell while the other differentiates into a primary spermatocyte.
-
Meiosis I: The primary spermatocyte (diploid) undergoes meiosis I, a reductional division, resulting in two secondary spermatocytes (haploid). This stage is crucial as it reduces the chromosome number by half, ensuring that upon fertilization, the zygote will have the correct diploid number of chromosomes. Crossing over occurs during this phase, leading to genetic recombination and increased genetic diversity among sperm cells.
-
Meiosis II: Each secondary spermatocyte undergoes meiosis II, an equational division, producing two haploid spermatids. This division further separates sister chromatids, resulting in four haploid cells from each primary spermatocyte.
-
Spermiogenesis: This is the final stage of spermatogenesis, a transformative process where spermatids differentiate into mature spermatozoa (sperm). This involves significant morphological changes:
- Formation of the acrosome: A cap-like structure at the head of the sperm, containing enzymes crucial for penetrating the ovum.
- Condensation of the nucleus: The genetic material is tightly packed, making the sperm head compact and streamlined.
- Development of the flagellum: A whip-like tail providing motility for sperm movement towards the ovum.
- Mitochondrial sheath formation: Mitochondria cluster around the flagellum, providing energy for motility.
Hormonal Regulation of Spermatogenesis:
The process is tightly regulated by hormones, primarily testosterone produced by the Leydig cells in the testes, under the influence of luteinizing hormone (LH) from the anterior pituitary gland. Follicle-stimulating hormone (FSH) also plays a crucial role, stimulating Sertoli cells to support spermatogenesis and produce inhibin, a hormone that negatively regulates FSH production through a feedback loop, maintaining hormonal balance.
Oogenesis: The Creation of the Ovum
Oogenesis, the process of ovum (egg) production, differs significantly from spermatogenesis. It's a discontinuous process that begins before birth, pauses, and resumes at puberty, ceasing at menopause. Unlike spermatogenesis, oogenesis produces only one functional gamete per meiosis cycle.
Stages of Oogenesis:
-
Prenatal Development: During fetal development, oogonia (diploid stem cells) multiply through mitosis. These oogonia then enter meiosis I, but arrest in prophase I, remaining dormant until puberty. These arrested cells are called primary oocytes.
-
Puberty and Follicular Development: At puberty, under the influence of follicle-stimulating hormone (FSH), a small number of primary oocytes are recruited each menstrual cycle. These oocytes complete meiosis I, producing a secondary oocyte (haploid) and a first polar body (haploid), a smaller cell that typically degenerates.
-
Ovulation and Meiosis II: The secondary oocyte proceeds to meiosis II but arrests in metaphase II. This arrested secondary oocyte is released from the ovary during ovulation.
-
Fertilization and Completion of Meiosis II: Meiosis II only completes if the secondary oocyte is fertilized by a sperm cell. Upon fertilization, the secondary oocyte completes meiosis II, producing a mature ovum (haploid) and a second polar body (haploid), which also usually degenerates. The mature ovum then fuses with the sperm, restoring the diploid chromosome number and initiating embryonic development.
Hormonal Regulation of Oogenesis:
Oogenesis is primarily regulated by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. FSH stimulates follicle development and growth, leading to the maturation of the primary oocyte. LH triggers ovulation, the release of the secondary oocyte from the mature follicle (Graafian follicle). Estrogen and progesterone, produced by the ovarian follicles and corpus luteum, also play crucial roles in the regulation of the menstrual cycle and oogenesis.
Comparing the Processes: A Detailed Analysis
The table below provides a more detailed comparison, highlighting the key distinctions between spermatogenesis and oogenesis:
| Feature | Spermatogenesis | Oogenesis |
|---|---|---|
| Timing | Continuous from puberty to death | Begins prenatally, pauses, and resumes at puberty; ceases at menopause |
| Location | Seminiferous tubules of the testes | Ovaries |
| Number of Gametes Produced | Four functional gametes (sperm) per meiosis | One functional gamete (ovum) and three polar bodies per meiosis |
| Cytoplasmic Division | Cytoplasm is divided equally among the four resulting spermatids | Cytoplasm is largely retained by the ovum, with minimal cytoplasm in polar bodies |
| Size of Gametes | Relatively small and motile | Relatively large and non-motile |
| Chromosome Number | Haploid (n) | Haploid (n) |
| Meiosis Completion | Continuous and complete | Meiosis I completes at puberty; Meiosis II only completes upon fertilization |
| Genetic Variation | High due to crossing over and independent assortment during meiosis | High due to crossing over during meiosis I (although crossing over is slightly reduced) |
| Hormonal Control | Primarily testosterone (influenced by LH and FSH) | Primarily FSH and LH (with roles for estrogen and progesterone) |
| Developmental Timing | Relatively short | Relatively long |
Clinical Significance: Implications of Differences
The differences between spermatogenesis and oogenesis have significant clinical implications:
-
Infertility: Disruptions in either spermatogenesis or oogenesis can lead to infertility. Male infertility can result from various factors affecting sperm production, motility, or morphology. Female infertility can arise from problems with ovulation, oocyte maturation, or fallopian tube function.
-
Genetic Disorders: Errors during meiosis can lead to aneuploidy (abnormal chromosome number), resulting in genetic disorders such as Down syndrome (trisomy 21) or Turner syndrome (XO). The higher frequency of aneuploidy in oocytes contributes to a higher risk of chromosomal abnormalities in older mothers.
-
Cancer Treatment: Chemotherapy and radiation therapy can impair both spermatogenesis and oogenesis, leading to infertility. Cryopreservation (freezing) of gametes before treatment is a potential solution to preserve fertility.
-
Assisted Reproductive Technologies (ART): ART techniques such as in-vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) overcome infertility by manipulating gametes outside the body. The understanding of spermatogenesis and oogenesis is essential for the development and success of these techniques.
Conclusion: A Tale of Two Gametogeneses
Spermatogenesis and oogenesis, while both essential for sexual reproduction, exhibit striking differences reflecting the distinct roles of male and female gametes. Spermatogenesis is a continuous process producing numerous small, motile sperm, while oogenesis is a discontinuous process producing a single, large, non-motile ovum per cycle. The hormonal regulation, timing, and cytological details of these processes vary greatly. Understanding these differences is crucial in various fields, including reproductive medicine, genetics, and developmental biology, offering insights into the complex mechanisms of human reproduction and paving the way for advancements in reproductive technologies and treatments for related disorders. Future research continues to unravel the intricate details of these processes, promising further breakthroughs in our understanding of human reproduction.
Latest Posts
Latest Posts
-
Distilled Water Does Not Conduct A Current
Mar 25, 2025
-
A Projectile Is Fired Horizontally From A Gun
Mar 25, 2025
-
Why Europe Is Called The Peninsula Of Peninsulas
Mar 25, 2025
-
Which Of The Following Is A Mineralocorticoid
Mar 25, 2025
-
Which Of The Following Is Not A Benefit Of Insurance
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about The Basic Difference Between Spermatogenesis And Oogenesis Is That . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
