Prevents Backflow Of Blood Into The Left Ventricle
News Leon
Mar 29, 2025 · 7 min read
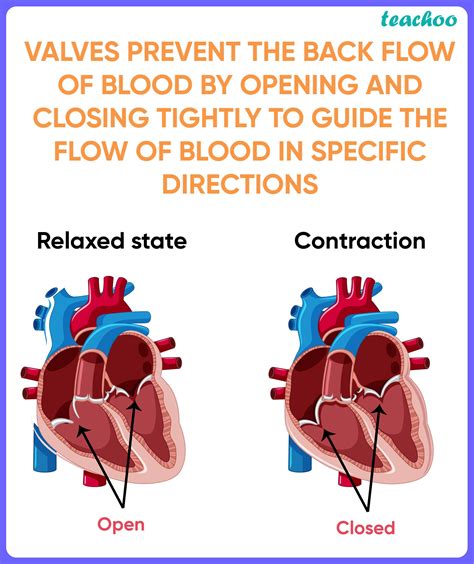
Table of Contents
Preventing Backflow of Blood into the Left Ventricle: A Deep Dive into Atrioventricular Valves
The human heart, a marvel of biological engineering, relies on a precise choreography of contractions and relaxations to efficiently pump blood throughout the body. Central to this intricate process are the heart valves, which act as one-way gates, ensuring unidirectional blood flow. This article delves deep into the mechanisms that prevent backflow of blood into the left ventricle, focusing primarily on the mitral valve's crucial role and the consequences of its malfunction.
The Mitral Valve: Guardian of the Left Ventricular Inlet
The mitral valve, also known as the bicuspid valve or left atrioventricular valve, is the primary gatekeeper preventing backflow from the left ventricle into the left atrium. Its strategic location between these two chambers is vital for maintaining the heart's efficient pumping action. Understanding its structure and function is paramount to comprehending how backflow is prevented.
Anatomy of the Mitral Valve: A Complex Structure
The mitral valve is composed of two leaflets or cusps – the anterior and posterior – that are tethered to the papillary muscles by chordae tendineae. These strong, fibrous cords act like guy-wires, preventing the leaflets from inverting or prolapsing into the left atrium during ventricular contraction (systole).
-
Leaflets: These are thin, but robust, flaps of tissue that open and close in a coordinated manner. Their intricate structure ensures a tight seal when closed, preventing regurgitation.
-
Papillary Muscles: These are muscular projections from the ventricular wall that provide crucial support to the chordae tendineae. Their contraction helps to stabilize the valve leaflets during ventricular systole.
-
Chordae Tendineae: These strong, collagenous cords connect the papillary muscles to the valve leaflets. They are essential for preventing leaflet prolapse and ensuring the valve's proper closure.
The Coordinated Dance of Valve Closure: A Symphony of Mechanics
The prevention of left ventricular backflow is not a passive process. It involves a carefully choreographed sequence of events that requires precise timing and coordination between the atria, ventricles, and the valvular apparatus.
-
Atrial Contraction (Atrial Systole): The left atrium contracts, pushing blood into the left ventricle. The mitral valve is open, allowing this blood flow.
-
Ventricular Filling: The left ventricle fills with blood, preparing for the forceful ejection of blood into the aorta.
-
Ventricular Contraction (Ventricular Systole): As the left ventricle contracts, the pressure within the ventricle rises dramatically. This increased pressure forces the mitral valve leaflets together, creating a tight seal.
-
Papillary Muscle Contraction: Simultaneously with ventricular contraction, the papillary muscles contract, tightening the chordae tendineae. This prevents the leaflets from being forced open into the left atrium.
-
Aortic Valve Opening: Once the pressure in the left ventricle surpasses the pressure in the aorta, the aortic valve opens, and blood is forcefully ejected into the systemic circulation.
-
Ventricular Relaxation (Diastole): As the left ventricle relaxes, the pressure within the ventricle falls below the pressure in the left atrium. This allows the mitral valve to passively open again, initiating the next cycle.
This precise orchestration ensures that blood flows unidirectionally from the left atrium to the left ventricle and then into the systemic circulation, preventing backflow at every stage.
Consequences of Mitral Valve Dysfunction: When the System Fails
When the mitral valve fails to function correctly, blood can leak back into the left atrium during ventricular contraction. This condition, known as mitral regurgitation, can have serious consequences.
Mitral Regurgitation: The Breakdown of the System
Several factors can contribute to mitral regurgitation:
-
Mitral Valve Prolapse: This occurs when the mitral valve leaflets bulge back into the left atrium during ventricular contraction. This is often caused by abnormalities in the valve leaflets or chordae tendineae.
-
Rheumatic Fever: This inflammatory condition can damage the mitral valve leaflets, leading to scarring and dysfunction.
-
Infective Endocarditis: Infection of the heart valves can damage the valve leaflets, impairing their ability to close properly.
-
Congenital Heart Defects: Some congenital heart defects can affect the mitral valve's structure and function.
-
Cardiomyopathy: Diseases affecting the heart muscle can weaken the papillary muscles, compromising the valve's support system.
The Impact of Mitral Regurgitation: A Cascade of Problems
Mitral regurgitation can lead to a number of complications, including:
-
Left Atrial Enlargement: The increased volume of blood in the left atrium due to backflow causes the atrium to enlarge over time.
-
Pulmonary Hypertension: The increased volume of blood in the left atrium can lead to increased pressure in the pulmonary veins and capillaries, resulting in pulmonary hypertension.
-
Heart Failure: The heart has to work harder to compensate for the backflow, leading to heart failure.
-
Atrial Fibrillation: The enlarged left atrium can be prone to atrial fibrillation, an irregular heartbeat.
-
Stroke: Atrial fibrillation increases the risk of blood clots forming in the left atrium, which can travel to the brain and cause a stroke.
Diagnostics and Management: Identifying and Addressing the Problem
Diagnosing mitral regurgitation often involves a combination of physical examination, electrocardiogram (ECG), echocardiogram, and other advanced imaging techniques.
Diagnostic Tools: Unveiling the Issue
-
Physical Examination: A doctor might detect a heart murmur, a swishing sound caused by turbulent blood flow due to regurgitation.
-
Electrocardiogram (ECG): An ECG can detect changes in the heart's rhythm and electrical activity associated with mitral regurgitation and its complications.
-
Echocardiogram: This is the gold standard for diagnosing mitral regurgitation. It uses ultrasound to visualize the heart's structure and function, providing detailed images of the mitral valve and identifying the degree of regurgitation.
-
Cardiac Catheterization: In some cases, cardiac catheterization might be used to measure pressures within the heart chambers and assess the severity of regurgitation.
Management Strategies: A Multifaceted Approach
Treatment for mitral regurgitation depends on its severity and the presence of symptoms. Management strategies include:
-
Lifestyle Modifications: These may involve dietary changes, weight management, and regular exercise to reduce the strain on the heart.
-
Medications: Medications can help manage symptoms such as heart failure and atrial fibrillation.
-
Surgical Intervention: For severe mitral regurgitation, surgical intervention, such as mitral valve repair or replacement, might be necessary to restore proper valve function. Mitral valve repair aims to restore the valve's natural function while preserving its native tissue. Mitral valve replacement involves replacing the damaged valve with a prosthetic valve.
Prevention: Proactive Measures for a Healthy Heart
While not all causes of mitral regurgitation are preventable, adopting a healthy lifestyle can significantly reduce the risk of developing heart conditions that can lead to valve dysfunction.
Lifestyle Choices that Protect Your Heart
-
Maintaining a Healthy Weight: Obesity increases the strain on the heart, increasing the risk of developing various heart conditions, including those that affect the mitral valve.
-
Regular Exercise: Regular physical activity strengthens the heart muscle and improves overall cardiovascular health.
-
Balanced Diet: A diet rich in fruits, vegetables, and whole grains and low in saturated and trans fats is crucial for maintaining heart health.
-
Managing Blood Pressure and Cholesterol: High blood pressure and cholesterol levels can damage blood vessels and increase the risk of heart disease.
-
Avoiding Smoking and Excessive Alcohol Consumption: Smoking and excessive alcohol intake damage the cardiovascular system, increasing the risk of heart conditions.
Conclusion: A Symphony of Function, a Call for Prevention
The prevention of backflow of blood into the left ventricle is a complex process relying on the intricate interplay of the mitral valve, papillary muscles, chordae tendineae, and the coordinated contractions of the heart chambers. Understanding the mechanisms involved in this crucial function highlights the importance of maintaining cardiovascular health through a healthy lifestyle. Early diagnosis and appropriate management of mitral valve dysfunction are essential to preventing the serious consequences of backflow and ensuring a healthy heart. By embracing a proactive approach to heart health and seeking timely medical attention when necessary, individuals can significantly reduce their risk of developing mitral valve problems and maintain a high quality of life.
Latest Posts
Latest Posts
-
Number Of Protons Neutrons And Electrons In Beryllium
Apr 01, 2025
-
What Is The Bond Order Of Li2
Apr 01, 2025
-
Is Baking Cookies A Chemical Or Physical Change
Apr 01, 2025
-
Which Type Of Electromagnetic Wave Has The Shortest Wavelength
Apr 01, 2025
-
Which Of The Following Is True About Monopolistic Competition
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Prevents Backflow Of Blood Into The Left Ventricle . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
