Parathyroid Hormone Does All Of The Following Except
News Leon
Apr 01, 2025 · 6 min read
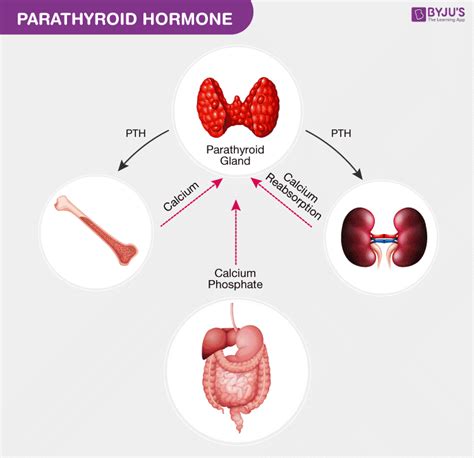
Table of Contents
Parathyroid Hormone: Actions and Exceptions
Parathyroid hormone (PTH), secreted by the parathyroid glands, is a crucial regulator of calcium and phosphorus homeostasis in the body. Its primary function is to maintain serum calcium levels within a narrow, tightly controlled range, essential for numerous physiological processes, including muscle contraction, nerve impulse transmission, and blood clotting. While PTH primarily elevates blood calcium, its effects are multifaceted and intricate. This article will delve into the various actions of PTH, highlighting the exception to its generally understood effects.
The Primary Actions of Parathyroid Hormone
PTH exerts its influence through various mechanisms, targeting several key organs and tissues:
1. Bone Resorption: Increasing Calcium Release
One of PTH's most significant actions is stimulating bone resorption. This process involves the breakdown of bone tissue, releasing calcium and phosphate ions into the bloodstream. PTH achieves this by activating osteoclasts, specialized cells responsible for bone resorption. Osteoclasts, upon stimulation by PTH, secrete acids and enzymes that dissolve the bone matrix, liberating calcium and phosphate. This action is crucial in raising serum calcium levels when they dip below the optimal range. The effect is not uniform across all bone types; PTH preferentially targets the cancellous bone (spongy bone) rather than the cortical bone (compact bone). The specific mechanisms involved in PTH-induced osteoclast activation are complex and involve interactions with various cell types and signaling pathways. These intricacies are still an active area of research in endocrinology.
2. Renal Calcium Reabsorption: Minimizing Calcium Excretion
PTH also acts on the kidneys, enhancing calcium reabsorption in the distal tubules. This process reduces the amount of calcium lost in the urine, further contributing to the maintenance of serum calcium levels. The precise mechanisms behind this renal effect of PTH involve modulating the expression and activity of specific calcium transporters within the renal tubules. These transporters actively move calcium from the filtrate back into the bloodstream. This renal effect, combined with the bone resorption effect, ensures that calcium is efficiently conserved and serum calcium levels remain stable.
3. Renal Phosphate Excretion: Regulating Phosphate Levels
While PTH's primary goal is calcium homeostasis, it also plays a role in phosphate metabolism. PTH inhibits phosphate reabsorption in the proximal tubules of the kidneys. This results in increased phosphate excretion in the urine, lowering serum phosphate levels. This action is crucial because elevated serum phosphate can interfere with calcium homeostasis and potentially lead to the formation of calcium phosphate precipitates. The balance between calcium and phosphate levels is delicately maintained, and PTH plays a critical role in this regulation. The reduction in serum phosphate induced by PTH is a secondary effect but is still significant in preventing adverse consequences of hyperphosphatemia.
4. Vitamin D Activation: Enhancing Calcium Absorption
PTH indirectly influences calcium absorption from the gut by stimulating the production of the active form of vitamin D, 1,25-dihydroxyvitamin D3 (calcitriol). Vitamin D is essential for calcium absorption in the intestines. PTH increases the activity of 1α-hydroxylase, the enzyme responsible for converting the inactive form of vitamin D (25-hydroxyvitamin D) into its active form, calcitriol. Calcitriol then enhances calcium absorption in the intestines. This action ensures a sufficient supply of calcium from the diet, contributing to the overall calcium balance. The interaction between PTH and vitamin D highlights the intricate interplay of hormones in regulating calcium metabolism.
The Exception: Parathyroid Hormone and Direct Stimulation of Osteoblasts
While PTH primarily stimulates osteoclasts to break down bone and release calcium, a nuance to its function exists. Initially, PTH binds to receptors on osteoblasts, the bone-forming cells. This interaction, however, does not directly lead to osteoblast activation in the same way it activates osteoclasts. Instead, the initial interaction of PTH with osteoblasts triggers a signaling cascade leading to the subsequent activation of osteoclasts. However, chronic exposure to high levels of PTH can lead to a different outcome. Prolonged and excessive PTH stimulation can, paradoxically, stimulate osteoblast activity, leading to bone formation. This is a crucial exception to the generally understood bone resorptive effect of PTH. This effect is particularly evident in the case of intermittent PTH therapy, which is used to treat osteoporosis.
Understanding the Intermittent PTH Therapy Exception
Intermittent PTH administration, unlike continuous high levels of PTH, promotes bone formation. The mechanism behind this anabolic effect is believed to involve several factors:
-
Differential receptor signaling: The intermittent nature of PTH administration allows for a different type of receptor engagement on osteoblasts, leading to the stimulation of bone formation rather than solely bone resorption. Continuous exposure seemingly desensitizes the beneficial pathway.
-
Increased osteoblast differentiation: Intermittent PTH administration may enhance the differentiation and proliferation of osteoblasts, leading to an increase in bone formation.
-
Reduced osteocyte apoptosis: PTH may also help to protect against osteocyte apoptosis (programmed cell death), contributing to bone mass preservation. Osteocytes play crucial roles in sensing mechanical loading and in maintaining bone homeostasis.
The clinical application of this exception is significant in the treatment of osteoporosis. Intermittent PTH therapy has been shown to be effective in increasing bone mineral density and reducing fracture risk in patients with osteoporosis. This demonstrates the clinical significance of understanding the nuanced effects of PTH on bone remodeling. The difference between continuous and intermittent administration highlights the complex interplay of timing and dosage in determining the ultimate physiological effect.
Clinical Significance and Disorders Related to Parathyroid Hormone
Understanding PTH's actions is crucial in diagnosing and managing various endocrine disorders. Abnormal PTH secretion can lead to significant health problems:
-
Hyperparathyroidism: This condition involves excessive PTH production, leading to elevated serum calcium levels (hypercalcemia), increased bone resorption, and potentially kidney stones. The excessive calcium can cause a range of symptoms, including fatigue, nausea, and muscle weakness.
-
Hypoparathyroidism: In contrast, insufficient PTH production results in decreased serum calcium levels (hypocalcemia) and potentially life-threatening complications such as seizures and cardiac arrhythmias. The symptoms can include muscle cramps, tingling sensations, and even tetany.
Precise diagnosis and management of these conditions require careful monitoring of serum calcium, phosphate, and PTH levels, along with appropriate treatment strategies. These strategies can involve medications to manage calcium levels, dietary adjustments, or in cases of severe hypoparathyroidism, hormone replacement therapy.
Conclusion: A Complex Regulator of Calcium Homeostasis
Parathyroid hormone is a pivotal regulator of calcium and phosphate homeostasis. While its primary function is to increase serum calcium levels through bone resorption and renal calcium reabsorption, it also plays a role in phosphate excretion and vitamin D activation. A key exception to its primarily catabolic role in bone is the anabolic effect observed with intermittent PTH administration, which has crucial therapeutic implications in osteoporosis treatment. Understanding the multifaceted actions of PTH and the exceptions to its generally understood effects is essential for the diagnosis and management of various endocrine disorders affecting calcium and bone metabolism. Further research continues to unravel the complexities of PTH signaling and its influence on bone remodeling, paving the way for improved therapeutic strategies targeting bone diseases.
Latest Posts
Latest Posts
-
How To Initialize A Tuple In Python
Apr 02, 2025
-
Find The Acceleration When The Velocity Is 0
Apr 02, 2025
-
Are Metals Solid At Room Temperature
Apr 02, 2025
-
Which Of The Following Statements Correctly Describes Gene Linkage
Apr 02, 2025
-
Complete The Complementary Strand Of Dna
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Parathyroid Hormone Does All Of The Following Except . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
