How Many Oxygen Can Hemoglobin Carry
News Leon
Mar 28, 2025 · 5 min read
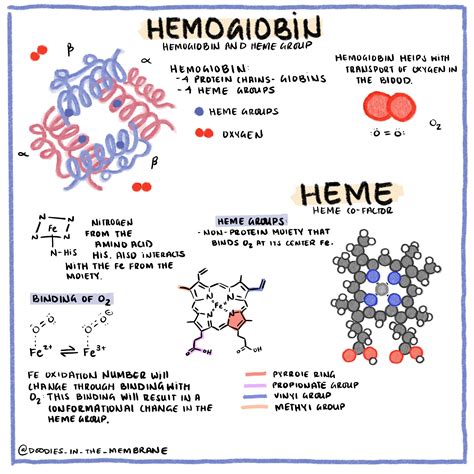
Table of Contents
How Much Oxygen Can Hemoglobin Carry? Understanding Oxygen Saturation and Transport
Oxygen is essential for life. Our bodies rely on a constant supply to fuel cellular respiration, the process that generates energy. The efficient transport of oxygen from the lungs to the tissues is crucial, and this is where hemoglobin, a remarkable protein found in red blood cells, plays a starring role. But how much oxygen can hemoglobin actually carry? This article delves deep into the fascinating world of hemoglobin's oxygen-carrying capacity, exploring the factors that influence it and the implications for overall health.
Understanding Hemoglobin's Structure and Function
Hemoglobin is a tetrameric protein, meaning it's composed of four subunits. Each subunit contains a heme group, a porphyrin ring complex containing a ferrous ion (Fe²⁺). This iron atom is the key player in oxygen binding. The four subunits are typically two alpha and two beta chains, although variations exist (e.g., fetal hemoglobin has two alpha and two gamma chains). This quaternary structure is crucial for hemoglobin's cooperative binding of oxygen.
The Cooperative Binding of Oxygen: A Closer Look
The binding of oxygen to one heme group induces a conformational change in the hemoglobin molecule, making it easier for subsequent oxygen molecules to bind to the remaining heme groups. This is known as cooperative binding, and it significantly increases the efficiency of oxygen uptake in the lungs and release in the tissues. This positive cooperativity is essential for the sigmoid shape of the oxygen-hemoglobin dissociation curve.
Calculating Hemoglobin's Oxygen-Carrying Capacity
The oxygen-carrying capacity of hemoglobin is typically expressed as the amount of oxygen that can be bound per gram of hemoglobin (gHb). A common measurement is the volume of oxygen bound per 100 mL of blood. Several factors influence this capacity:
1. The Number of Hemoglobin Molecules:
The more hemoglobin molecules present in the blood, the greater the oxygen-carrying capacity. This is directly related to the hematocrit (the percentage of red blood cells in blood). Anemia, a condition characterized by a low red blood cell count, significantly reduces the oxygen-carrying capacity of the blood.
2. The Availability of Oxygen:
The partial pressure of oxygen (PO₂) in the environment surrounding the hemoglobin plays a crucial role. In the lungs, where PO₂ is high, hemoglobin readily binds oxygen. In the tissues, where PO₂ is lower, oxygen is released. This difference in PO₂ is the driving force behind oxygen transport.
3. Hemoglobin's Affinity for Oxygen:
Hemoglobin's affinity for oxygen is influenced by several factors, including:
- pH: A decrease in pH (acidosis) reduces hemoglobin's affinity for oxygen, promoting oxygen release to the tissues. This is known as the Bohr effect.
- Temperature: Increased temperature also reduces hemoglobin's affinity for oxygen, facilitating oxygen unloading in metabolically active tissues.
- 2,3-Bisphosphoglycerate (2,3-BPG): This molecule binds to hemoglobin, reducing its oxygen affinity. Levels of 2,3-BPG increase during conditions like hypoxia (low oxygen levels) to enhance oxygen delivery to tissues.
- Carbon Dioxide: Increased carbon dioxide levels reduce hemoglobin's affinity for oxygen. This is also part of the Bohr effect.
4. Altitude and Oxygen Saturation
At higher altitudes, the partial pressure of oxygen is lower. This results in lower oxygen saturation of hemoglobin. The body adapts to this by increasing red blood cell production (polycythemia) to compensate for the reduced oxygen-carrying capacity per red blood cell.
Oxygen Saturation: A Key Indicator
Oxygen saturation (SpO₂) refers to the percentage of hemoglobin molecules carrying oxygen. It's typically measured using a pulse oximeter, a non-invasive device that uses light absorption to estimate the oxygen saturation of arterial blood. A normal SpO₂ is typically between 95% and 100%. Values below this range indicate hypoxemia, a condition of low blood oxygen levels.
Factors Affecting Oxygen Transport Beyond Hemoglobin
While hemoglobin is the primary oxygen transporter, other factors contribute to efficient oxygen transport:
- Cardiac Output: The heart's ability to pump blood efficiently impacts oxygen delivery to tissues. Reduced cardiac output can lead to insufficient oxygen supply.
- Blood Flow: Adequate blood flow to the tissues is crucial for oxygen delivery. Vascular diseases can impair blood flow, compromising oxygen transport.
- Tissue Metabolism: The rate of oxygen consumption by the tissues also influences oxygen levels. Highly metabolically active tissues require a greater oxygen supply.
Clinical Implications of Altered Oxygen-Carrying Capacity
Several conditions can affect hemoglobin's oxygen-carrying capacity, leading to significant health consequences:
- Anemia: Reduced red blood cell count or hemoglobin levels lead to decreased oxygen-carrying capacity, causing fatigue, shortness of breath, and other symptoms.
- Carbon Monoxide Poisoning: Carbon monoxide binds to hemoglobin with much greater affinity than oxygen, preventing oxygen from binding and causing severe hypoxia.
- Sickle Cell Anemia: Abnormal hemoglobin (hemoglobin S) causes red blood cells to become sickle-shaped, impairing their ability to carry oxygen and leading to various complications.
- Thalassemia: A group of inherited disorders characterized by reduced or absent globin chain synthesis, resulting in decreased hemoglobin production and reduced oxygen-carrying capacity.
- Methemoglobinemia: This condition involves the oxidation of the iron in hemoglobin from Fe²⁺ to Fe³⁺, rendering it unable to bind oxygen.
Measuring Hemoglobin and Oxygen Saturation: Diagnostic Tests
Several diagnostic tests are used to assess hemoglobin levels and oxygen saturation:
- Complete Blood Count (CBC): This routine blood test measures hemoglobin levels, red blood cell count, and other parameters.
- Pulse Oximetry: This non-invasive method measures oxygen saturation using a sensor placed on a finger or toe.
- Arterial Blood Gas (ABG) analysis: This more invasive test directly measures blood oxygen levels, carbon dioxide levels, and pH.
Conclusion: The Crucial Role of Hemoglobin in Oxygen Transport
Hemoglobin's role in oxygen transport is paramount to life. Its remarkable ability to bind and release oxygen efficiently, coupled with its cooperative binding properties, allows for the effective delivery of oxygen to the body's tissues. Understanding the factors that influence hemoglobin's oxygen-carrying capacity, such as oxygen partial pressure, pH, temperature, and 2,3-BPG levels, is crucial for comprehending various physiological processes and clinical conditions. Maintaining adequate hemoglobin levels and ensuring efficient oxygen transport are essential for overall health and well-being. Regular health check-ups and monitoring of relevant parameters can help identify and address potential issues early on, preventing serious complications. While the exact amount of oxygen a single hemoglobin molecule can carry is dependent on the aforementioned factors, its overall contribution to oxygen transport in the human body is undeniable and vital for survival. Further research continues to unravel the intricacies of hemoglobin function and its impact on human health.
Latest Posts
Latest Posts
-
Calculate Zeff For A Valence Electron In An Oxygen Atom
Mar 31, 2025
-
Reaction Between Magnesium And Hydrochloric Acid
Mar 31, 2025
-
Is Electric Charge A Vector Quantity
Mar 31, 2025
-
Which Statement About Equations And Expressions Is True
Mar 31, 2025
-
Points On The Same Line Are Called
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about How Many Oxygen Can Hemoglobin Carry . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
