What Is The Principal Cation Of The Ecf
News Leon
Mar 20, 2025 · 5 min read
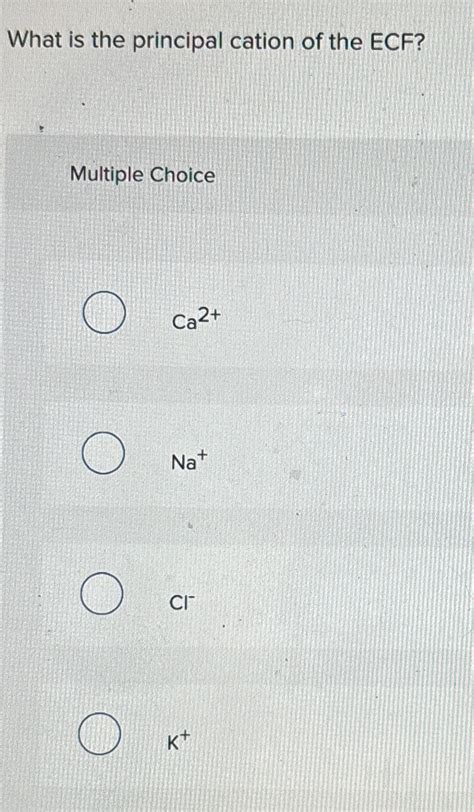
Table of Contents
What is the Principal Cation of the ECF? Understanding Sodium's Crucial Role
The extracellular fluid (ECF) is the vital fluid environment surrounding cells, crucial for nutrient delivery and waste removal. Understanding its composition is paramount to comprehending human physiology. While many ions contribute to the ECF's complex balance, one reigns supreme: sodium (Na⁺). This article delves into the significance of sodium as the principal cation of the ECF, exploring its functions, regulation, and the consequences of imbalances.
Sodium: The Dominant Player in ECF
The extracellular fluid is a dynamic environment, a complex solution containing various electrolytes. These electrolytes are crucial for maintaining osmotic pressure, nerve impulse transmission, muscle contraction, and countless other physiological processes. Among these electrolytes, cations (positively charged ions) and anions (negatively charged ions) exist in a delicate equilibrium. While several cations reside in the ECF, including potassium (K⁺), calcium (Ca²⁺), and magnesium (Mg²⁺), sodium (Na⁺) is the dominant cation, overwhelmingly exceeding the concentrations of other positive ions. This dominance dictates its outsized influence on ECF properties and overall bodily function.
The Significance of Sodium's High Concentration
The significantly higher concentration of sodium in the ECF compared to the intracellular fluid (ICF) is no accident; it's essential for several key physiological roles:
-
Maintaining Osmotic Pressure: Sodium, alongside chloride (Cl⁻), is a major contributor to the ECF's osmotic pressure. This pressure is the force that draws water across semipermeable membranes. The high concentration of sodium in the ECF helps to maintain the proper fluid balance between the ECF and ICF. Deviations from this balance, as seen in dehydration or overhydration, profoundly impact cellular function.
-
Fluid Volume Regulation: Sodium plays a critical role in regulating blood volume. Changes in sodium concentration trigger the renin-angiotensin-aldosterone system (RAAS), a hormonal cascade influencing kidney function and water retention. This ensures blood volume remains within a healthy range.
-
Nerve Impulse Transmission: Sodium is fundamental to the generation and propagation of nerve impulses. The rapid influx of sodium ions into nerve cells triggers depolarization, the crucial step initiating the action potential that transmits nerve signals.
-
Muscle Contraction: Similar to nerve impulse transmission, sodium ions play a vital role in muscle contraction. The influx of sodium ions is essential for initiating the process of muscle fiber depolarization, leading to muscle contraction.
-
Nutrient Absorption: Sodium actively participates in the absorption of nutrients from the digestive tract. It is involved in the co-transport mechanisms that facilitate the uptake of glucose and amino acids.
Sodium Regulation: A Complex Balancing Act
Maintaining the precise balance of sodium in the ECF is a tightly controlled process involving several organs and hormones. The kidneys are the primary regulators, constantly adjusting sodium excretion based on the body's needs.
The Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a complex hormonal system that plays a pivotal role in regulating sodium balance. When blood volume or blood pressure drops, or when sodium levels are low, the kidneys release renin. Renin catalyzes a cascade of reactions ultimately leading to the production of aldosterone. Aldosterone acts on the kidneys to increase sodium reabsorption and potassium excretion. This action conserves sodium, increasing blood volume and pressure.
Antidiuretic Hormone (ADH)
Another crucial player is antidiuretic hormone (ADH), also known as vasopressin. ADH is released from the pituitary gland in response to dehydration or increased blood osmolarity. It promotes water reabsorption in the kidneys, further concentrating sodium in the ECF and restoring fluid balance.
Atrial Natriuretic Peptide (ANP)
Conversely, when blood volume and pressure are high, the heart releases atrial natriuretic peptide (ANP). ANP inhibits sodium reabsorption in the kidneys, leading to increased sodium excretion in the urine. This helps to lower blood volume and pressure.
Consequences of Sodium Imbalance
Disruptions to sodium homeostasis can have severe consequences, ranging from mild symptoms to life-threatening conditions.
Hyponatremia (Low Sodium Levels)
Hyponatremia occurs when the concentration of sodium in the blood is abnormally low. Causes range from excessive water intake to conditions affecting kidney function. Symptoms can include nausea, vomiting, headache, confusion, and, in severe cases, seizures and coma.
Hypernatremia (High Sodium Levels)
Hypernatremia results from an abnormally high concentration of sodium in the blood. This is often due to dehydration or conditions affecting sodium excretion. Symptoms can include thirst, lethargy, confusion, seizures, and coma. The severity is directly related to the rapidity and degree of the increase in sodium concentration.
The Interplay of Sodium with Other Electrolytes
The importance of sodium doesn't exist in isolation; it's intricately linked to the balance of other electrolytes. For instance, the sodium-potassium pump, a vital transmembrane protein, maintains the concentration gradient of sodium and potassium across cell membranes. This pump is essential for nerve impulse transmission and muscle contraction. Furthermore, the balance between sodium and calcium is important for proper muscle function and blood clotting.
Clinical Significance and Diagnostic Tests
Understanding sodium's role is critical for medical professionals. Diagnosing and managing sodium imbalances requires accurate measurement of serum sodium levels through blood tests. Treatment strategies vary depending on the cause and severity of the imbalance, ranging from fluid management to medication.
Dietary Considerations and Sodium Intake
Dietary sodium intake significantly impacts ECF sodium levels. Excessive sodium consumption, often through processed foods and table salt, can contribute to hypertension and other health problems. Maintaining a balanced diet with moderate sodium intake is crucial for overall health.
Conclusion: Sodium's Indispensable Role in Human Physiology
In conclusion, sodium is the undisputed principal cation of the extracellular fluid. Its high concentration is not merely a coincidence but a fundamental requirement for numerous physiological processes. Maintaining the delicate balance of sodium in the ECF is a tightly regulated process involving the kidneys, hormones, and other electrolytes. Disruptions to this balance can lead to severe health consequences. Understanding sodium's crucial role is essential for maintaining health and treating related medical conditions. From its involvement in fluid balance and osmotic pressure to its critical functions in nerve impulse transmission and muscle contraction, sodium's impact spans the breadth of human physiology, making it an electrolyte of paramount importance. Further research continues to elucidate the intricacies of sodium regulation and its interactions with other components of the complex biological system that is the human body. This ongoing investigation highlights the ongoing need for careful management of sodium intake and the vigilant monitoring of sodium levels for the maintenance of optimal health.
Latest Posts
Latest Posts
-
Activation Energy For The Forward Reaction
Mar 20, 2025
-
Under What Conditions Are Gases Most Likely To Behave Ideally
Mar 20, 2025
-
Which Of The Following Is A Non Phagocytic Cell
Mar 20, 2025
-
Ball A Of Mass 5 0 Kilograms
Mar 20, 2025
-
Hiv Is Considered To Be A Retrovirus Because
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about What Is The Principal Cation Of The Ecf . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
