Tissue That Forms The Inner Lining Of Our Mouth
News Leon
Mar 16, 2025 · 7 min read
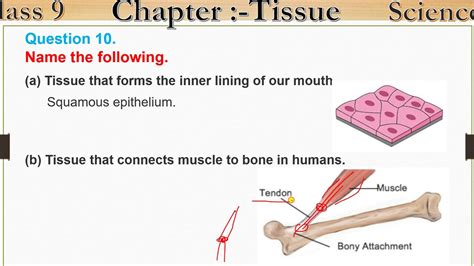
Table of Contents
The Oral Mucosa: A Deep Dive into the Tissue Lining Your Mouth
The seemingly simple lining of your mouth, the oral mucosa, is a marvel of biological engineering. Far from being just a passive barrier, this tissue plays a crucial role in numerous vital functions, from taste and speech to the initial stages of digestion and immune defense. Understanding its structure, function, and potential pathologies is essential for appreciating its significance in overall health. This comprehensive article will explore the intricacies of the oral mucosa, covering its composition, different types, functions, and common conditions affecting it.
Composition and Layers of the Oral Mucosa
The oral mucosa is a specialized type of mucous membrane, a type of epithelial tissue that lines various body cavities. Unlike skin, it is constantly moist due to the secretion of saliva. Its structure is characterized by three main layers:
1. Epithelium: The Protective Outer Layer
The epithelium is the outermost layer, acting as the primary barrier against the external environment. It's primarily composed of stratified squamous epithelium, meaning it's made of multiple layers of flat, scale-like cells. This layered structure provides exceptional protection against mechanical stress from chewing, swallowing, and speaking. The type of epithelium varies depending on the specific location within the oral cavity.
-
Keratinized epithelium: Found in areas subjected to high friction, like the gingiva (gums) and hard palate (roof of the mouth). Keratin, a tough protein, strengthens and waterproofs these areas, enhancing their resistance to abrasion. Keratinization provides exceptional protection against mechanical wear and tear.
-
Non-keratinized epithelium: Lines areas with less friction, such as the buccal mucosa (lining of the cheeks), labial mucosa (lining of the lips), floor of the mouth, and ventral surface of the tongue. It's softer and more permeable than keratinized epithelium. This allows for greater absorption of certain substances and easier interaction with sensory receptors.
2. Lamina Propria: The Supportive Connective Tissue
Beneath the epithelium lies the lamina propria, a layer of connective tissue. It's composed of collagen and elastin fibers, blood vessels, nerves, and immune cells. These components provide structural support to the epithelium, supply it with nutrients, and facilitate wound healing. The lamina propria's rich vascular network is essential for the delivery of oxygen and nutrients to the overlying epithelium and the removal of waste products. The presence of immune cells plays a crucial role in defending against pathogens that might enter through the oral mucosa. The density and organization of the connective tissue vary across different regions of the oral cavity.
3. Submucosa: Deeper Connective Tissue (In Some Areas)
In some areas of the oral cavity, a third layer, the submucosa, exists beneath the lamina propria. This layer is composed of loose connective tissue, adipose tissue (fat), and often contains salivary glands and blood vessels. The submucosa allows for some degree of movement and flexibility of the overlying mucosa. Its presence is particularly noticeable in areas like the cheeks and lips, contributing to their mobility. The absence of the submucosa in areas like the gingiva accounts for its firmer attachment to the underlying bone.
Types of Oral Mucosa
The oral mucosa isn't uniform throughout the mouth; it's categorized into different types based on its structure and function:
-
Masticatory mucosa: This is the toughest type, found on the gingiva and hard palate. It's characterized by its thick keratinized epithelium and dense lamina propria firmly bound to the underlying periosteum (bone covering). This firm attachment is crucial for withstanding the forces of mastication (chewing). Its primary function is protection.
-
Lining mucosa: This type lines the cheeks, lips, floor of the mouth, and ventral surface of the tongue. It's characterized by its non-keratinized epithelium, a less dense lamina propria, and often a well-defined submucosa. This type of mucosa is more flexible and pliable, allowing for movement during speech and swallowing. Its functions include protection and lubrication.
-
Specialized mucosa: This unique type covers the dorsal surface (upper surface) of the tongue. It's characterized by the presence of taste buds, which are responsible for the sense of taste. The specialized mucosa also contains numerous papillae, which provide texture and enhance the tongue’s interaction with food. Its primary function is gustation (taste perception).
Functions of the Oral Mucosa
The oral mucosa performs a multitude of critical functions:
-
Protection: This is its primary function, acting as a barrier against physical, chemical, and microbial insults. The keratinized epithelium of the masticatory mucosa is particularly robust in protecting against mechanical wear and tear.
-
Sensation: The rich innervation of the oral mucosa allows for detection of temperature, pressure, pain, and taste. Sensory receptors in the epithelium and lamina propria transmit these signals to the brain, enabling us to perceive our environment and the food we consume.
-
Secretion: Salivary glands within the mucosa secrete saliva, which lubricates the mouth, aids in digestion, and helps maintain oral hygiene. The constant moisture provided by saliva prevents dryness and cracking of the mucosa.
-
Absorption: While less permeable than the intestinal mucosa, the oral mucosa can absorb certain substances, including medications applied directly to the mucosa (e.g., sublingual medications). This route of administration allows for rapid entry of medications into the bloodstream.
-
Immune Defense: The oral mucosa houses a substantial number of immune cells, which play a vital role in defending against pathogens. These immune cells are crucial for preventing infections and maintaining oral health.
-
Speech and Mastication: The flexibility and mobility of the oral mucosa are essential for clear speech and efficient chewing. The proper functioning of the oral mucosa contributes greatly to oral health and overall well-being.
Common Conditions Affecting the Oral Mucosa
Several conditions can affect the health and integrity of the oral mucosa. These include:
-
Aphthous ulcers (canker sores): These are small, painful ulcers that frequently occur on the non-keratinized mucosa. Their exact cause is unknown, but stress, trauma, and immune responses are potential contributing factors.
-
Oral thrush (candidiasis): A fungal infection caused by Candida albicans, often appearing as white patches on the mucosa. It's more common in individuals with weakened immune systems or those using antibiotics.
-
Oral lichen planus: A chronic inflammatory condition of unknown cause, presenting as white lacy lesions or erosions on the mucosa.
-
Leukoplakia: White patches on the mucosa that can't be easily scraped off. While most cases are benign, some can be precancerous lesions.
-
Oral mucositis: Inflammation and ulceration of the oral mucosa, often a side effect of chemotherapy or radiation therapy.
-
Gingivitis and periodontitis: Inflammatory conditions of the gingiva (gums) that can lead to tooth loss if left untreated.
-
Oral cancer: While relatively uncommon, it's a serious condition that can affect any area of the oral mucosa. Early detection and treatment are crucial for improving prognosis.
Maintaining Oral Mucosal Health
Maintaining healthy oral mucosa requires consistent effort and good oral hygiene practices:
-
Regular brushing and flossing: Removes food particles and plaque, reducing the risk of infections and gum disease.
-
Healthy diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains supports overall health, including oral mucosal health.
-
Hydration: Drinking plenty of water keeps the mucosa moist and prevents dryness and cracking.
-
Stress management: Reducing stress can help prevent the development of conditions like aphthous ulcers.
-
Regular dental checkups: Allows for early detection and treatment of any abnormalities or conditions affecting the oral mucosa.
-
Avoiding irritants: Minimizing exposure to tobacco, alcohol, and other potential irritants can help protect the oral mucosa.
Conclusion: The Unsung Hero of Oral Health
The oral mucosa, a seemingly simple tissue, plays a surprisingly significant role in our overall health and well-being. Its intricate structure and multiple functions highlight its importance in protection, sensation, secretion, and immune defense. Understanding its composition, different types, and potential pathologies empowers us to better appreciate its crucial contribution to oral and systemic health. By practicing good oral hygiene and seeking professional dental care when needed, we can safeguard the health of this often-overlooked, yet vitally important, tissue. Regular check-ups with a dentist or oral surgeon are paramount in early detection of any potential issues, ensuring optimal oral health. The proactive approach towards maintaining the health of your oral mucosa is essential for a healthy and fulfilling life.
Latest Posts
Latest Posts
-
Which Of The Following Is Polynomial
Mar 17, 2025
-
Is Boiling Water A Physical Change
Mar 17, 2025
-
Is A Webcam An Input Or Output Device
Mar 17, 2025
-
Word For A Person Who Uses Big Words
Mar 17, 2025
-
What Is 375 As A Percentage
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Tissue That Forms The Inner Lining Of Our Mouth . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
