The Type Of Epithelium That Lines The Urinary Bladder
News Leon
Mar 25, 2025 · 6 min read
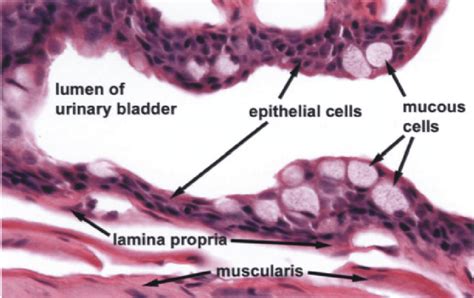
Table of Contents
The Epithelium Lining the Urinary Bladder: A Deep Dive into Urothelium
The urinary bladder, a crucial component of the urinary system, is responsible for storing urine before its elimination from the body. The remarkable ability of the bladder to expand significantly to accommodate varying urine volumes and then recoil to its original size is largely due to the unique properties of its lining: urothelium, also known as transitional epithelium. This article delves into the intricate structure, function, and clinical significance of this specialized epithelium.
Understanding Urothelium: Structure and Composition
Urothelium is a stratified epithelium, meaning it's composed of multiple layers of cells. Unlike other stratified epithelia, however, its appearance changes dramatically depending on the bladder's state of distension. When the bladder is empty, the urothelium appears thicker and folded, while in a distended state, it thins and flattens considerably, showcasing its remarkable adaptability.
Layers of Urothelium:
The urothelium consists of three main layers:
-
Basal Layer: This deepest layer comprises a single row of cuboidal or columnar cells resting on the basement membrane. These cells are mitotically active, responsible for the regeneration and maintenance of the urothelium.
-
Intermediate Layer: This layer, composed of several layers of polyhedral or pear-shaped cells, provides structural support and contributes to the overall thickness of the epithelium. Cell junctions, such as desmosomes and adherens junctions, are crucial for maintaining the integrity of this layer and preventing leaks.
-
Superficial Layer: The most distinctive layer, the superficial layer consists of large, umbrella-shaped cells known as umbrella cells. These cells are unique and play a critical role in the bladder's impermeability to urine. Their apical surface is characterized by specialized structures called asymmetric unit membranes (AUMs), which form a continuous, impermeable barrier. These AUMs are crucial for preventing the back-diffusion of water and small molecules, ensuring efficient urine storage. The unique lipid composition of these membranes and the presence of tight junctions between umbrella cells are vital for maintaining the bladder's barrier function.
Specialized Cell Junctions: Maintaining Integrity and Function
The tight junctions between umbrella cells are essential for the urothelium's barrier function. These junctions create a seal that restricts the passage of substances between cells, preventing the leakage of urine components into the underlying tissues. Furthermore, the adherens junctions and desmosomes provide strong cell-to-cell adhesion, contributing to the overall mechanical strength and resilience of the urothelium. This robust cellular architecture is essential to withstand the distension and relaxation cycles the bladder undergoes during urine storage and voiding.
The Role of Glycocalyx: A Protective Shield
The apical surface of the umbrella cells is covered by a thick layer of glycocalyx, a complex carbohydrate-rich layer that acts as a protective shield. This glycocalyx protects the underlying cells from the potentially harmful components of urine, such as toxins, pathogens, and acidic pH. Furthermore, the glycocalyx plays a role in mediating cell-cell and cell-matrix interactions.
Function of Urothelium: Beyond a Simple Barrier
The function of urothelium extends far beyond simply acting as a passive barrier. It plays a critical role in several key processes:
Protection Against Urine Components:
As mentioned earlier, the urothelium protects the underlying tissues from the potentially damaging effects of urine. The impermeability of the AUMs and the protective glycocalyx shield the bladder wall from the harmful effects of urea, uric acid, and other urinary components.
Maintaining Fluid Balance:
The urothelium plays a significant role in regulating fluid balance. The tight junctions between umbrella cells restrict the passage of water and ions, preventing excessive fluid loss from the bladder into the surrounding tissues. This precise control over fluid permeability is crucial for maintaining the integrity of the urinary system.
Sensory Perception:
The urothelium is not merely a passive barrier; it also contains sensory nerve endings that detect bladder distension. These sensory receptors transmit signals to the central nervous system, triggering the urge to urinate when the bladder reaches a certain level of fullness. This sensory function is critical for maintaining urinary continence and preventing urinary incontinence.
Immune Response:
The urothelium participates in the immune response by acting as a first line of defense against invading pathogens. It expresses various immune-related molecules that can detect and respond to pathogens, such as bacteria and viruses. The immune response of the urothelium contributes to the overall defense of the urinary tract against infection.
Regeneration and Repair:
Urothelium possesses a remarkable capacity for regeneration and repair. The basal layer's actively dividing cells continuously replace damaged or worn-out cells, ensuring the maintenance of the urothelium's integrity and function. This inherent regenerative capability is crucial for the bladder's ability to withstand repeated cycles of distension and relaxation.
Clinical Significance of Urothelial Dysfunction
Dysfunction of the urothelium can lead to various clinical conditions, highlighting the importance of its proper function:
Urinary Tract Infections (UTIs):
Compromised urothelial integrity, for example, due to damage or inflammation, can increase the risk of UTIs. A breach in the barrier function of the urothelium allows bacteria to penetrate the underlying tissues, leading to infection.
Interstitial Cystitis (IC)/Bladder Pain Syndrome (BPS):
IC/BPS is a chronic bladder condition characterized by pelvic pain, urinary frequency, and urgency. It is believed that abnormalities in the urothelium, including altered permeability and inflammation, play a significant role in the development of IC/BPS. Research indicates dysfunction in the tight junctions and altered expression of various molecules might be involved.
Bladder Cancer:
Most bladder cancers originate from the urothelium. The exact causes are complex and not fully understood, but factors such as smoking, exposure to certain chemicals, and chronic irritation or inflammation are implicated. The study of urothelial changes and alterations in cellular processes is crucial for understanding the pathogenesis and developing improved diagnostic and treatment strategies for bladder cancer.
Other Urothelial-Related Conditions:
Other conditions associated with urothelial dysfunction include:
- Urolithiasis: Kidney stones can cause damage to the urothelium as they pass through the urinary tract.
- Radiation cystitis: Radiation therapy can damage the urothelium, leading to inflammation and other complications.
- Chemical cystitis: Exposure to irritants or toxins can also damage the urothelium.
Research and Future Directions
Ongoing research continues to unravel the intricacies of urothelium and its role in health and disease. Areas of active investigation include:
- Improved understanding of the molecular mechanisms underlying urothelial regeneration and repair: This knowledge could lead to the development of novel therapies for bladder injuries and diseases.
- Development of better diagnostic tools for detecting urothelial dysfunction: This is essential for early diagnosis and treatment of conditions like bladder cancer and IC/BPS.
- Identification of new therapeutic targets for treating urothelial-related disorders: This could involve strategies to enhance urothelial barrier function, reduce inflammation, or stimulate regeneration.
- Exploring the role of urothelium in mediating interactions between the urinary system and the immune system: This understanding could contribute to the development of new treatments for UTIs and other infections of the urinary tract.
Conclusion
The urothelium lining the urinary bladder is far more than just a passive barrier; it's a highly specialized and dynamic tissue crucial for efficient urine storage, protection against harmful substances, and sensory perception. Its remarkable adaptability, sophisticated cell junctions, and inherent regenerative capacity are all essential for maintaining the health and function of the urinary system. Further research into the intricacies of urothelium will undoubtedly lead to significant advances in the diagnosis and treatment of urological diseases. Understanding its complex structure and function is critical for improving patient care and advancing the field of urology.
Latest Posts
Latest Posts
-
Which Characteristic Is Common To All Chordates
Mar 28, 2025
-
Give The Major Product For The Following Reaction
Mar 28, 2025
-
Is India In The Northern Or Southern Hemisphere
Mar 28, 2025
-
Predict The Major Product S Of The Following Reaction
Mar 28, 2025
-
Find The Value Of X In The Figure Below
Mar 28, 2025
Related Post
Thank you for visiting our website which covers about The Type Of Epithelium That Lines The Urinary Bladder . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
