Serous Membrane That Covers The Lungs
News Leon
Mar 17, 2025 · 7 min read
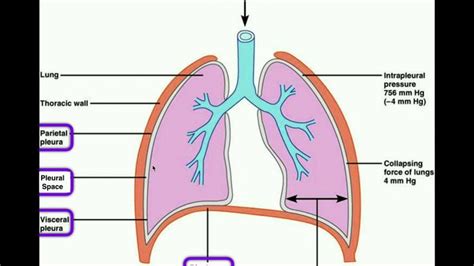
Table of Contents
The Pleura: A Comprehensive Guide to the Serous Membrane Covering the Lungs
The lungs, the vital organs responsible for gas exchange, are not simply nestled within the ribcage. They are enveloped by a delicate yet crucial serous membrane known as the pleura. Understanding the pleura's structure, function, and clinical significance is paramount to comprehending respiratory physiology and pathology. This comprehensive guide delves into the intricacies of this essential membrane, exploring its anatomy, physiology, and common associated diseases.
Anatomy of the Pleura: Layers and Spaces
The pleura is a thin, double-layered serous membrane. This means it's composed of a single layer of mesothelial cells overlying a thin layer of connective tissue. These two layers are separated by a potential space, the pleural cavity, which, under normal physiological conditions, contains only a small amount of lubricating serous fluid. The two layers are:
1. Visceral Pleura: The Lung's Embrace
The visceral pleura is intimately attached to the surface of the lungs, dipping into the fissures that separate the lobes. It's essentially inseparable from the lung parenchyma itself. Its delicate nature allows it to follow the lung's movements during inspiration and expiration without friction. The visceral pleura is richly supplied with sensory nerve fibers, primarily from the vagus nerve, though pain sensation is minimal under normal conditions.
2. Parietal Pleura: The Chest Wall Lining
The parietal pleura lines the thoracic cavity, adhering to the inner surface of the ribcage, the diaphragm, the mediastinum (the space between the lungs containing the heart and other organs), and the superior mediastinum. Unlike the visceral pleura, the parietal pleura receives innervation from somatic nerves, making it sensitive to pain, pressure, and temperature changes. This difference in innervation is clinically significant, as pleural pain can be quite severe in certain conditions.
The Pleural Cavity: A Lubricated Space
Between the visceral and parietal pleura lies the pleural cavity, a potential space containing a small amount of serous fluid (approximately 10-15 ml). This fluid acts as a lubricant, minimizing friction during respiratory movements. The pressure within the pleural cavity is typically subatmospheric (negative pressure), which plays a crucial role in maintaining lung inflation. This negative pressure is created by the opposing elastic recoil forces of the lungs and the chest wall.
Physiology of the Pleura: Breathing and Pressure
The pleura's primary function is to facilitate efficient lung inflation and deflation during respiration. This function is inextricably linked to the negative pleural pressure:
1. Negative Pressure and Lung Expansion:
During inspiration, the diaphragm contracts and flattens, and the intercostal muscles expand the ribcage. This increases the volume of the thoracic cavity. Because the pleural cavity is sealed, the increase in volume leads to a decrease in pleural pressure, becoming even more negative. This negative pressure difference between the pleural cavity and the lung's interior draws air into the lungs.
2. Surface Tension and Lung Compliance:
The serous fluid in the pleural cavity also reduces surface tension between the visceral and parietal pleura. This significantly reduces friction during respiratory movements, enhancing lung compliance (the ease with which the lungs can expand). Without this lubricating effect, lung expansion would be significantly more difficult and energy-consuming.
3. Protection and Compartmentalization:
The pleura provides a protective barrier around the lungs, shielding them from external trauma and infection. The pleural cavity also acts as a compartmentalizing structure, helping to localize infections or fluid accumulation, preventing their spread throughout the chest cavity.
Clinical Significance of Pleural Diseases: A Spectrum of Conditions
The pleura's intimate relationship with the lungs and the thoracic cavity makes it susceptible to a wide range of diseases. These conditions can dramatically affect respiratory function and overall health.
1. Pleuritis (Pleurisy): Inflammation of the Pleura
Pleuritis, also known as pleurisy, is an inflammation of the pleura. It's often characterized by sharp, stabbing chest pain, particularly worsened by deep breaths or coughing. Pleuritis can be caused by various factors, including:
- Infections: Viral, bacterial, or fungal infections can inflame the pleura.
- Autoimmune diseases: Conditions like lupus or rheumatoid arthritis can lead to pleuritis.
- Cancer: Lung cancer or cancers that spread to the pleura (metastatic disease).
- Pulmonary embolism: A blood clot in the lung's blood vessels.
- Trauma: Injury to the chest wall or lungs.
The pain associated with pleuritis arises from the inflammation irritating the parietal pleura's sensitive nerve endings.
2. Pleural Effusion: Fluid Buildup in the Pleural Cavity
Pleural effusion is the accumulation of excess fluid in the pleural cavity. This can be due to a variety of causes, including:
- Congestive heart failure: Fluid buildup due to the heart's inability to pump efficiently.
- Pneumonia: Infection in the lungs.
- Cancer: Spread of cancer cells to the pleura.
- Liver disease: Cirrhosis can cause fluid retention.
- Kidney disease: Nephrotic syndrome can lead to fluid buildup.
The type of fluid in the pleural effusion can provide clues to the underlying cause. For example, a transudate (watery fluid) is often associated with congestive heart failure, while an exudate (protein-rich fluid) is more commonly seen in infections or cancers.
3. Pneumothorax: Collapsed Lung
A pneumothorax is a condition where air enters the pleural cavity, leading to lung collapse. This can occur spontaneously (due to lung blebs or cysts), traumatically (due to chest injuries), or iatrogenically (due to medical procedures). The entry of air into the pleural cavity equalizes the pressure within the pleural cavity and the atmosphere, eliminating the negative pressure crucial for lung expansion. This leads to partial or complete lung collapse.
4. Mesothelioma: A Rare and Aggressive Cancer
Mesothelioma is a rare and aggressive cancer that arises from the mesothelial cells lining the pleura. It's strongly linked to asbestos exposure. Diagnosis is typically challenging, and the prognosis is often poor due to the cancer's rapid spread and resistance to treatment.
5. Pleural Thickening: Fibrosis of the Pleural Tissues
Pleural thickening refers to the thickening and scarring of the pleural tissues. This is frequently associated with chronic inflammation, asbestos exposure, or prior pleural infections. The thickened pleura can restrict lung expansion and reduce respiratory function.
Diagnostic Techniques for Pleural Diseases
Accurate diagnosis of pleural diseases often requires a combination of imaging techniques and diagnostic procedures.
1. Chest X-Ray: Initial Imaging
A chest X-ray is the initial imaging study used to evaluate pleural diseases. It can reveal the presence of pleural effusions, pneumothorax, or pleural thickening.
2. Computed Tomography (CT) Scan: Detailed Visualization
A CT scan provides more detailed images of the chest, allowing for better visualization of pleural abnormalities and their extent. CT scans can help differentiate between different types of pleural effusions and identify underlying lung pathology.
3. Ultrasound: Guided Procedures
Ultrasound is frequently used to guide diagnostic procedures like thoracentesis (removing pleural fluid for analysis). It's particularly helpful in identifying the best location for needle insertion to minimize risks.
4. Thoracentesis: Fluid Removal and Analysis
Thoracentesis involves inserting a needle into the pleural cavity to remove fluid for analysis. This allows for the determination of the fluid's characteristics (transudate vs. exudate), cytological examination (for cancer cells), and microbiological analysis (for infections).
5. Pleural Biopsy: Tissue Sample
A pleural biopsy involves obtaining a tissue sample from the pleura for pathological examination. This is particularly useful in the diagnosis of pleural cancers and other conditions where tissue analysis is required for definitive diagnosis.
Conclusion: The Vital Role of the Pleura
The pleura, though a seemingly simple serous membrane, plays a vital role in respiratory physiology and is closely intertwined with a variety of clinical conditions. A comprehensive understanding of its anatomy, physiology, and associated pathologies is crucial for healthcare professionals involved in the diagnosis and management of chest diseases. This detailed knowledge contributes to accurate diagnosis, prompt treatment, and ultimately, improved patient outcomes. Continued research continues to refine our understanding of pleural diseases and advance the development of effective treatment strategies.
Latest Posts
Latest Posts
-
0 3 To The Power Of 3
Mar 17, 2025
-
What Is 5 Percent Of 200
Mar 17, 2025
-
What Is The 5 Difference Between Photosynthesis And Respiration
Mar 17, 2025
-
Which Of The Following Is A Characteristic Of Cnidarians
Mar 17, 2025
-
Metallic Trends In The Periodic Table
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Serous Membrane That Covers The Lungs . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
