Prevents Backflow Into The Left Ventricle.
News Leon
Mar 28, 2025 · 6 min read
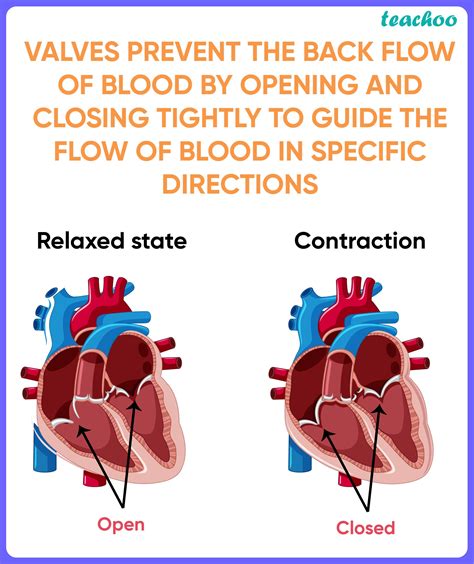
Table of Contents
- Prevents Backflow Into The Left Ventricle.
- Table of Contents
- Preventing Backflow into the Left Ventricle: A Comprehensive Guide
- The Aortic Valve: The Primary Guardian Against Left Ventricular Backflow
- Anatomy and Physiology of the Aortic Valve
- Conditions Leading to Aortic Valve Dysfunction
- Compensatory Mechanisms and Clinical Manifestations
- Diagnosis and Treatment of Aortic Regurgitation
- Maintaining Cardiovascular Health: Proactive Steps for Aortic Valve Function
- Conclusion: A Complex Interplay of Structure and Function
- Latest Posts
- Latest Posts
- Related Post
Preventing Backflow into the Left Ventricle: A Comprehensive Guide
The heart, a tireless engine driving our circulatory system, relies on a delicate balance of pressure and valve function to ensure efficient blood flow. A critical aspect of this efficiency is the prevention of backflow, particularly the retrograde movement of blood from the aorta back into the left ventricle. This backflow, if unchecked, can severely compromise cardiac output and lead to various cardiovascular complications. This article delves into the intricate mechanisms that prevent this backflow, exploring the anatomy, physiology, and pathology involved.
The Aortic Valve: The Primary Guardian Against Left Ventricular Backflow
The primary structure preventing backflow from the aorta into the left ventricle is the aortic valve. This crucial valve is positioned at the exit of the left ventricle, acting as a one-way door allowing blood to flow from the heart into the aorta during systole (contraction) while preventing its return during diastole (relaxation).
Anatomy and Physiology of the Aortic Valve
The aortic valve is composed of three cusps, also known as leaflets, which are semi-lunar in shape. These cusps are made of connective tissue, primarily collagen and elastin, covered by a thin layer of endothelium. During ventricular contraction, the pressure within the left ventricle rises, forcing the cusps open and allowing blood to surge into the aorta. As the ventricle relaxes, the pressure in the aorta exceeds that in the ventricle, causing the cusps to close, preventing backflow.
The precise closing mechanism relies on several factors:
- Pressure Gradient: The most significant factor is the pressure difference between the aorta and the left ventricle. A healthy pressure gradient ensures that the aortic valve closes tightly, preventing regurgitation.
- Cusps' Shape and Coaptation: The shape and flexibility of the cusps are crucial for proper coaptation (close contact). Any irregularity in cusp shape or flexibility can compromise the seal, leading to leakage.
- Papillary Muscles and Chordae Tendineae: Although not directly involved in aortic valve closure, the papillary muscles and chordae tendineae play an indirect role. These structures support the mitral valve (located between the left atrium and left ventricle), preventing prolapse which could indirectly influence aortic valve function.
Conditions Leading to Aortic Valve Dysfunction
Several conditions can compromise the efficacy of the aortic valve, leading to aortic regurgitation (backflow of blood into the left ventricle):
- Aortic Valve Stenosis: While primarily causing obstruction of blood flow out of the left ventricle, severe stenosis can indirectly affect the valve's ability to close properly.
- Aortic Valve Regurgitation: This is the direct consequence of the aortic valve failing to close completely. Causes include:
- Bicuspid Aortic Valve: A congenital condition where the valve has only two cusps instead of three, leading to structural weakness and potential regurgitation.
- Rheumatic Heart Disease: A condition resulting from rheumatic fever, causing inflammation and scarring of the valve leaflets.
- Infective Endocarditis: Infection of the valve leaflets, causing damage and dysfunction.
- Connective Tissue Disorders: Conditions like Marfan syndrome can weaken the aortic valve, making it prone to regurgitation.
- Aortic Dissection: A tear in the aortic wall can compromise the valve's function.
- Degeneration: Age-related degeneration of the valve leaflets can lead to calcification and stiffening, impairing closure.
Compensatory Mechanisms and Clinical Manifestations
The body possesses inherent compensatory mechanisms to mitigate the effects of mild to moderate aortic regurgitation. These include:
- Increased Stroke Volume: The heart attempts to compensate for the backflow by increasing the amount of blood pumped with each beat. This increases cardiac output to maintain adequate tissue perfusion.
- Increased Heart Rate: The heart increases its rate to compensate for the reduced effective blood volume in the aorta.
However, if the regurgitation is severe or the compensatory mechanisms are insufficient, several clinical manifestations can arise:
- Heart Murmur: A characteristic diastolic murmur (heard during heart relaxation) is often present due to the backflow of blood into the left ventricle.
- Chest Pain: Increased workload on the heart can lead to angina (chest pain).
- Shortness of Breath: Congestive heart failure can occur as the heart struggles to maintain adequate blood flow, causing shortness of breath, particularly during exertion.
- Fatigue: The increased cardiac workload can lead to fatigue and reduced exercise tolerance.
- Elevated Blood Pressure: Initially, there might be increased systolic blood pressure; however, in advanced stages, low blood pressure can also occur.
Diagnosis and Treatment of Aortic Regurgitation
Diagnosis of aortic regurgitation typically involves:
- Physical Examination: Auscultation (listening to the heart sounds) is crucial for detecting a diastolic murmur.
- Echocardiogram: This non-invasive imaging technique provides detailed images of the heart, allowing visualization of the aortic valve and assessment of the severity of regurgitation.
- Chest X-ray: Can reveal signs of heart enlargement associated with chronic aortic regurgitation.
- Cardiac Catheterization: A more invasive procedure that might be used in specific cases to further assess the severity and plan for surgery.
Treatment options vary depending on the severity of the regurgitation and the presence of symptoms:
- Medical Management: For mild cases, medications may be prescribed to manage symptoms such as hypertension and heart failure.
- Surgical Intervention: For moderate to severe cases, surgery may be necessary. Options include:
- Aortic Valve Replacement: Replacing the diseased valve with a mechanical or biological prosthetic valve.
- Aortic Valve Repair: In some cases, the valve can be repaired instead of replaced. This procedure is less invasive and often preferred when possible.
- Transcatheter Aortic Valve Replacement (TAVR): A minimally invasive procedure where a new valve is implanted via a catheter, avoiding open-heart surgery.
Maintaining Cardiovascular Health: Proactive Steps for Aortic Valve Function
Prevention and early detection are crucial in managing potential issues with the aortic valve and preventing backflow into the left ventricle. Maintaining a healthy lifestyle is essential:
- Regular Exercise: Maintaining a healthy weight through regular physical activity strengthens the cardiovascular system.
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains supports overall health and reduces the risk of cardiovascular disease.
- Blood Pressure Control: Managing hypertension through lifestyle modifications or medication is crucial.
- Cholesterol Management: Maintaining healthy cholesterol levels minimizes the risk of atherosclerosis, which can affect the aortic valve.
- Smoking Cessation: Smoking significantly increases the risk of cardiovascular diseases, including aortic valve disease.
Conclusion: A Complex Interplay of Structure and Function
Preventing backflow into the left ventricle is a critical function of the cardiovascular system, primarily managed by the aortic valve. Understanding the anatomy, physiology, and pathology of this valve is crucial for appreciating the complex interplay of structures and functions that maintain efficient blood flow. While the aortic valve plays the central role, the intricate interplay between pressure gradients, cusp morphology, and compensatory mechanisms contributes to its overall effectiveness. Early diagnosis and appropriate management, combined with a proactive approach to cardiovascular health, are vital in maintaining the integrity of the aortic valve and preventing debilitating backflow. Maintaining a healthy lifestyle and seeking prompt medical attention for any concerning symptoms are crucial steps towards ensuring the long-term health of the heart and its remarkable ability to sustain life.
Latest Posts
Latest Posts
-
Weak Acid And Weak Base Ph
Apr 01, 2025
-
What Is The Measure Of Angle B In Degrees
Apr 01, 2025
-
What Is The Formula Of Iq
Apr 01, 2025
-
A Path That An Electric Current Follows Is A
Apr 01, 2025
-
Distance From Earth To Sun Scientific Notation
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Prevents Backflow Into The Left Ventricle. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
