Diabetes Insipidus Is Caused By Hyposecretion Of
News Leon
Mar 18, 2025 · 7 min read
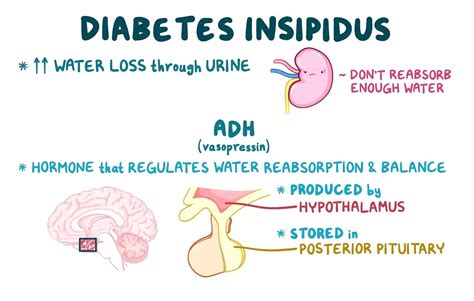
Table of Contents
- Diabetes Insipidus Is Caused By Hyposecretion Of
- Table of Contents
- Diabetes Insipidus: Caused by Hyposecretion of Vasopressin (ADH)
- Understanding the Role of Vasopressin (ADH)
- The Mechanism of Action: A Deeper Dive
- Types of Diabetes Insipidus: Central vs. Nephrogenic
- 1. Central Diabetes Insipidus (CDI): The Hyposecretion Problem
- 2. Nephrogenic Diabetes Insipidus (NDI): Kidney Resistance
- Symptoms of Diabetes Insipidus
- Diagnosing Diabetes Insipidus
- Managing Diabetes Insipidus
- Treatment for Central Diabetes Insipidus (CDI)
- Treatment for Nephrogenic Diabetes Insipidus (NDI)
- Living With Diabetes Insipidus: Long-Term Considerations
- Conclusion: Understanding the Hyposecretion Connection
- Latest Posts
- Latest Posts
- Related Post
Diabetes Insipidus: Caused by Hyposecretion of Vasopressin (ADH)
Diabetes insipidus (DI) is a rare disorder marked by the excretion of large amounts of severely diluted urine, leading to excessive thirst and frequent urination. Unlike diabetes mellitus, DI isn't related to blood sugar levels. Instead, it stems from a problem with the body's ability to regulate fluid balance, specifically due to a deficiency in vasopressin, also known as antidiuretic hormone (ADH). This article will delve into the causes, symptoms, diagnosis, and management of diabetes insipidus, focusing on the hyposecretion of vasopressin as its central etiology.
Understanding the Role of Vasopressin (ADH)
Vasopressin, produced in the hypothalamus of the brain, is a crucial hormone that plays a pivotal role in maintaining fluid balance. It acts primarily on the kidneys, influencing the reabsorption of water from the urine back into the bloodstream. When the body is dehydrated, the hypothalamus detects this and signals the pituitary gland to release more vasopressin. This increased vasopressin levels stimulate the kidneys to reabsorb more water, concentrating the urine and reducing the volume excreted. In essence, vasopressin helps the body conserve water.
The Mechanism of Action: A Deeper Dive
Vasopressin achieves its water-reabsorbing effect by binding to specific receptors (V2 receptors) located in the collecting ducts of the kidneys. This binding triggers a cascade of intracellular events that ultimately lead to the insertion of aquaporin-2 water channels into the cell membranes of the collecting duct cells. These channels act like tiny pores, allowing water to flow freely from the urine into the surrounding bloodstream, thus concentrating the urine. Without sufficient vasopressin, these aquaporin channels remain largely inactive, resulting in the excretion of large volumes of dilute urine—the hallmark of diabetes insipidus.
Types of Diabetes Insipidus: Central vs. Nephrogenic
Diabetes insipidus is broadly classified into two main types, primarily differentiated by the location of the underlying problem:
1. Central Diabetes Insipidus (CDI): The Hyposecretion Problem
Central diabetes insipidus is the most common type, directly related to the insufficient production or release of vasopressin from the hypothalamus or pituitary gland. This hyposecretion can arise from several causes:
-
Damage to the Hypothalamus or Pituitary Gland: This can occur due to:
- Head trauma: Accidents or injuries affecting the brain can damage the vasopressin-producing regions.
- Brain surgery: Procedures in the vicinity of the hypothalamus or pituitary gland can unintentionally disrupt vasopressin production or release.
- Tumors: Benign or malignant tumors can compress or destroy the hypothalamic-pituitary axis.
- Infections: Meningitis or encephalitis can inflame and damage the brain, affecting vasopressin production.
- Autoimmune disorders: In rare cases, the body's immune system may mistakenly attack the hypothalamus or pituitary gland, leading to decreased vasopressin production.
- Genetic mutations: Inherited genetic defects can affect the synthesis or release of vasopressin.
-
Idiopathic CDI: In some cases, no identifiable cause for the vasopressin deficiency can be found, and the condition is termed idiopathic CDI.
2. Nephrogenic Diabetes Insipidus (NDI): Kidney Resistance
Nephrogenic diabetes insipidus, in contrast to CDI, arises from the kidneys' inability to respond properly to vasopressin, even if sufficient amounts are produced and released. This resistance can be caused by several factors:
- Genetic mutations: Inherited mutations in the genes responsible for the vasopressin receptor (V2 receptor) or the aquaporin-2 water channels can impair the kidneys' response to vasopressin.
- Kidney disease: Chronic kidney diseases, such as polycystic kidney disease, can damage the kidney tubules, reducing their ability to reabsorb water.
- Medications: Certain medications, such as lithium (commonly used to treat bipolar disorder), demeclocycline (an antibiotic), and some amphotericin B formulations, can interfere with the action of vasopressin in the kidneys.
- Electrolyte imbalances: Severe imbalances in electrolytes, such as hypercalcemia (high calcium levels) and hypokalemia (low potassium levels), can impair the kidneys' response to vasopressin.
Symptoms of Diabetes Insipidus
The primary symptoms of DI, regardless of the underlying cause, stem from the excessive loss of water in the urine:
- Polyuria: The hallmark of DI is the excretion of abnormally large volumes of dilute urine (polyuria). Individuals may urinate several liters per day.
- Polydipsia: The body attempts to compensate for the fluid loss by triggering intense thirst (polydipsia). Individuals often feel constantly thirsty and drink copious amounts of fluids.
- Nocturia: Frequent nighttime urination (nocturia) is common, disrupting sleep.
- Dehydration: If fluid intake doesn't keep pace with the urine output, dehydration can occur, leading to symptoms like fatigue, weakness, dizziness, and even hypotension (low blood pressure).
- Infants and Children: In infants and young children, DI can lead to failure to thrive, poor weight gain, and developmental delays.
Diagnosing Diabetes Insipidus
Diagnosing DI involves a combination of tests aimed at evaluating the urine and assessing the body's response to vasopressin:
- Water deprivation test: This is a crucial diagnostic test. The patient is deprived of fluids for several hours while urine volume and concentration are monitored. The inability to concentrate urine during water deprivation strongly suggests DI.
- Vasopressin stimulation test: After a water deprivation test, synthetic vasopressin is administered. If the urine concentration increases significantly, it suggests CDI (the kidneys can respond to vasopressin). A lack of response indicates NDI (kidney resistance to vasopressin).
- Blood tests: Blood tests are performed to assess electrolyte levels, blood urea nitrogen (BUN), and creatinine levels, which help rule out other conditions and assess the severity of dehydration.
- Imaging studies: In cases suspected CDI, MRI or CT scans of the brain may be performed to identify any abnormalities in the hypothalamus or pituitary gland.
- Genetic testing: Genetic testing may be recommended to identify specific gene mutations responsible for NDI or familial forms of CDI.
Managing Diabetes Insipidus
The management of DI focuses on replacing the missing vasopressin or addressing the kidney's resistance to it:
Treatment for Central Diabetes Insipidus (CDI)
- Desmopressin (DDAVP): This is the most common treatment for CDI. It's a synthetic analogue of vasopressin that acts on the V2 receptors in the kidneys, promoting water reabsorption. It can be administered as a nasal spray, tablets, or injection. Dosage is tailored to individual needs.
- Underlying condition treatment: If CDI is secondary to another condition (e.g., a tumor), treating that underlying condition is crucial.
Treatment for Nephrogenic Diabetes Insipidus (NDI)
- Managing underlying conditions: Addressing underlying kidney diseases or electrolyte imbalances is paramount. Discontinuing medications that interfere with vasopressin action may also help.
- Lifestyle changes: Increasing fluid intake and following a low-sodium diet may help reduce urine output.
- Thiazide diuretics: Ironically, certain low-dose thiazide diuretics, despite being diuretics, may be beneficial in some cases of NDI, possibly by increasing the concentration of calcium in the kidneys and subtly enhancing water reabsorption.
- Amiloride: This potassium-sparing diuretic may help in some cases.
- Non-pharmacological approaches: Regular fluid intake and mindful hydration practices are vital for preventing dehydration and managing symptoms.
Living With Diabetes Insipidus: Long-Term Considerations
Living with DI requires ongoing vigilance and management. Regular monitoring of fluid intake and urine output is essential, especially during periods of illness or increased activity. Carrying a readily available source of fluids is advisable to prevent dehydration. Patients should also be aware of the potential side effects of their medications and seek medical attention for any concerning symptoms. Regular check-ups with an endocrinologist or nephrologist (depending on the type of DI) are necessary to monitor the condition's progression and adjust treatment as needed.
Conclusion: Understanding the Hyposecretion Connection
Diabetes insipidus, characterized by excessive thirst and urination, is fundamentally a disorder of fluid balance directly linked to the hyposecretion of vasopressin. Understanding the role of this critical hormone, the various causes of vasopressin deficiency or kidney resistance, and the diverse approaches to diagnosis and treatment is crucial for effective management of this condition. Early diagnosis and appropriate treatment are vital for improving the quality of life for individuals affected by DI and preventing serious complications associated with dehydration and electrolyte imbalances. This comprehensive understanding is key to empowering patients to proactively manage their condition and lead fulfilling lives. Remember, regular consultations with medical professionals are crucial for optimizing long-term management strategies.
Latest Posts
Latest Posts
-
Area Of An 8 Inch Circle
Mar 19, 2025
-
Which Of The Following Is True Of Iron
Mar 19, 2025
-
Python Check If A String Is A Number
Mar 19, 2025
-
What Is The Length Of Line Segment Pq
Mar 19, 2025
-
Homologous Chromosomes Separate During Which Phase Of Meiosis
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Diabetes Insipidus Is Caused By Hyposecretion Of . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
