What Is The Structural And Functional Unit Of Kidney
News Leon
Mar 23, 2025 · 7 min read
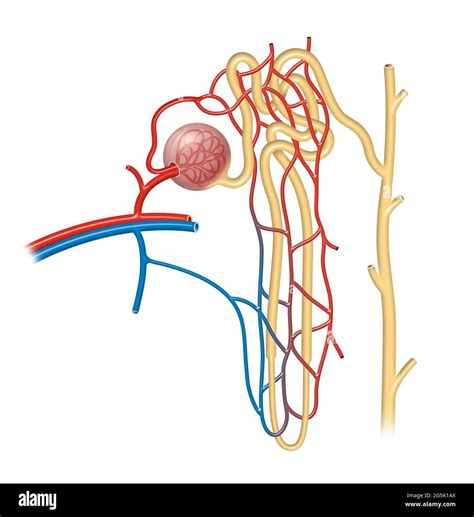
Table of Contents
What is the Structural and Functional Unit of the Kidney?
The human kidney, a remarkable organ, plays a vital role in maintaining overall health and homeostasis. Its primary function is to filter blood, removing waste products and excess fluids while conserving essential substances like electrolytes and nutrients. Understanding the intricate workings of the kidney requires delving into its fundamental building block: the nephron. This article will explore the nephron in detail, examining its structure, its crucial functional components, and the complex processes that occur within it to ensure proper kidney function.
The Nephron: The Workhorse of the Kidney
The nephron is the structural and functional unit of the kidney. Thousands of nephrons, intricately interwoven within the kidney's architecture, work tirelessly to perform the essential task of blood filtration and waste excretion. Each nephron consists of two main parts:
1. The Renal Corpuscle (Malpighian Body): The Filtration Site
The renal corpuscle is the initial segment of the nephron, responsible for the crucial first step in urine formation: glomerular filtration. It comprises two structures:
-
The Glomerulus: This is a network of highly specialized capillaries, forming a tuft-like structure. The glomerular capillaries are fenestrated, meaning they possess pores that allow for the passage of water and small solutes while effectively preventing the filtration of larger molecules like proteins and blood cells. The high pressure within the glomerulus is essential for driving the filtration process.
-
Bowman's Capsule (Glomerular Capsule): This cup-shaped structure surrounds the glomerulus. Its inner layer, composed of specialized epithelial cells called podocytes, plays a crucial role in regulating the filtration process. Podocytes possess foot-like processes that interdigitate, creating filtration slits that further refine the filtrate. The filtrate, now devoid of large proteins and blood cells, enters the next segment of the nephron.
2. The Renal Tubule: Fine-Tuning the Filtrate
The renal tubule is a long, convoluted structure extending from Bowman's capsule. It's responsible for modifying the initial filtrate, reabsorbing essential substances back into the bloodstream, and secreting additional waste products. The renal tubule is divided into several distinct segments, each contributing uniquely to the overall process:
-
Proximal Convoluted Tubule (PCT): The PCT is the longest and most active segment of the renal tubule. It's characterized by its brush border, composed of microvilli that significantly increase its surface area for reabsorption. Here, the majority of reabsorption occurs, including vital nutrients like glucose, amino acids, and water, along with essential electrolytes like sodium, potassium, and bicarbonate. The PCT also actively secretes certain substances, such as hydrogen ions and drugs.
-
Loop of Henle (Nephron Loop): This hairpin-shaped structure extends from the PCT and descends into the renal medulla before ascending back to the cortex. The loop of Henle plays a critical role in establishing an osmotic gradient within the medulla, which is essential for concentrating urine. The descending limb is permeable to water but relatively impermeable to solutes, while the ascending limb is impermeable to water but actively transports sodium and chloride ions out of the filtrate. This countercurrent mechanism allows for the efficient reabsorption of water and the concentration of urine.
-
Distal Convoluted Tubule (DCT): The DCT is shorter than the PCT and plays a critical role in fine-tuning the composition of the filtrate. It's primarily involved in regulating the reabsorption of sodium, potassium, calcium, and water under the influence of hormones like aldosterone and parathyroid hormone. It also secretes additional substances, such as potassium and hydrogen ions.
-
Collecting Duct: While not technically part of the nephron, the collecting duct is crucial in the final processing of urine. Multiple nephrons empty their filtrate into the collecting duct, which descends through the medulla. Here, the final adjustments to water reabsorption are made, influenced primarily by antidiuretic hormone (ADH). ADH increases water permeability in the collecting duct, leading to the reabsorption of more water and the production of more concentrated urine.
The Process of Urine Formation: A Step-by-Step Guide
Urine formation is a complex multi-step process that involves glomerular filtration, tubular reabsorption, and tubular secretion.
1. Glomerular Filtration: The Initial Sieve
Glomerular filtration is a passive process driven by the glomerular filtration pressure (GFP). GFP is determined by the balance between glomerular capillary blood pressure, Bowman's capsule hydrostatic pressure, and glomerular capillary oncotic pressure. This pressure difference forces water and small solutes from the glomerular capillaries into Bowman's capsule, forming the filtrate. The filtration membrane, composed of the fenestrated endothelium of the glomerular capillaries, the glomerular basement membrane, and the podocyte filtration slits, acts as a selective barrier, preventing the passage of large molecules like proteins and blood cells.
2. Tubular Reabsorption: Reclaiming the Essentials
Tubular reabsorption is the process by which essential substances, initially filtered into the Bowman's capsule, are reabsorbed back into the bloodstream from the renal tubules. This process involves both passive and active transport mechanisms. In the PCT, the majority of glucose, amino acids, and electrolytes are reabsorbed. Water reabsorption is primarily passive, driven by osmotic gradients established by solute reabsorption. The loop of Henle plays a critical role in establishing a concentration gradient in the medulla, allowing for efficient water reabsorption in the collecting duct.
3. Tubular Secretion: Refining the Waste Stream
Tubular secretion is an active process that involves the transport of certain substances from the peritubular capillaries into the renal tubules. This is a crucial process for eliminating waste products that were not effectively filtered in the glomerulus, as well as for regulating the pH of the blood. Hydrogen ions, potassium ions, and drugs are actively secreted into the renal tubules.
Hormonal Regulation: Maintaining the Balance
The process of urine formation is tightly regulated by several hormones:
-
Antidiuretic Hormone (ADH): Released by the posterior pituitary gland, ADH increases the permeability of the collecting duct to water, leading to increased water reabsorption and the production of concentrated urine.
-
Aldosterone: Secreted by the adrenal cortex, aldosterone stimulates the reabsorption of sodium ions in the DCT and collecting duct. This leads to increased water reabsorption and increased blood volume.
-
Parathyroid Hormone (PTH): Released by the parathyroid glands, PTH promotes calcium reabsorption in the DCT.
-
Atrial Natriuretic Peptide (ANP): Released by the heart in response to increased blood volume, ANP inhibits sodium reabsorption in the DCT, leading to increased sodium excretion and decreased blood volume.
Types of Nephrons: Juxtamedullary vs. Cortical
Nephrons are classified into two types based on their location within the kidney and the length of their loop of Henle:
-
Cortical Nephrons: These are the most abundant type of nephron, located primarily in the cortex. They have short loops of Henle that extend only slightly into the medulla.
-
Juxtamedullary Nephrons: These nephrons have long loops of Henle that extend deep into the medulla. They play a crucial role in establishing the osmotic gradient necessary for concentrating urine.
Clinical Significance: Understanding Kidney Diseases
Understanding the structure and function of the nephron is crucial for comprehending various kidney diseases. Damage to nephrons, often caused by infections, autoimmune diseases, or toxins, can lead to impaired kidney function, resulting in conditions like chronic kidney disease (CKD) and kidney failure. Many kidney diseases directly affect the filtration process, reabsorption, or secretion within the nephron, impacting the body's ability to maintain fluid and electrolyte balance and to eliminate waste products. Early detection and treatment of kidney diseases are vital to preventing irreversible damage.
Conclusion: The Nephron's Crucial Role in Health
The nephron, the structural and functional unit of the kidney, is a remarkably complex structure responsible for maintaining homeostasis and overall health. Its intricate mechanisms of filtration, reabsorption, and secretion ensure the efficient removal of waste products and the precise regulation of essential substances within the body. A thorough understanding of the nephron's architecture and function is essential for appreciating the vital role the kidneys play in maintaining health and for comprehending the impact of kidney diseases. Further research continually unveils more intricate details about the nephron's complex processes, offering promising avenues for the development of improved diagnostic and therapeutic strategies for kidney diseases.
Latest Posts
Latest Posts
-
When Is Marginal Cost At Its Minimum
Mar 25, 2025
-
Why Is Respiration Considered An Exothermic Reaction Class 10
Mar 25, 2025
-
An Amusement Park Ride Consists Of
Mar 25, 2025
-
What Shapes Do Not Have A Line Of Symmetry
Mar 25, 2025
-
The Distance Between One Crets And Another
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about What Is The Structural And Functional Unit Of Kidney . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
