Vessels That Contain Valves To Prevent Backflow Of Blood
News Leon
Mar 25, 2025 · 7 min read
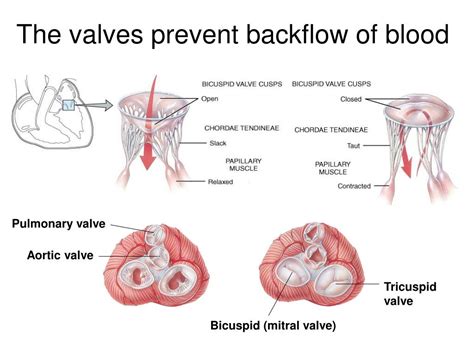
Table of Contents
Vessels That Contain Valves to Prevent Backflow of Blood: A Comprehensive Overview
The circulatory system, a marvel of biological engineering, relies on efficient unidirectional blood flow. This crucial aspect is ensured by a network of specialized vessels equipped with valves – tiny, yet powerful structures that prevent the backflow of blood, maintaining the vital pressure gradients necessary for efficient circulation. This article delves into the detailed anatomy, physiology, and clinical significance of these valved vessels, focusing primarily on veins and the lymphatic system.
The Role of Valves in Blood Circulation
The heart, the tireless pump of the circulatory system, propels blood through arteries, capillaries, and finally, veins. While arteries maintain relatively high pressure, venous pressure is significantly lower. This lower pressure poses a significant challenge: gravity. Without a mechanism to counteract the pull of gravity, blood would simply pool in the lower extremities, hindering efficient return to the heart. This is where venous valves step in. These one-way valves, strategically placed within veins, prevent backflow, ensuring that blood flows steadily towards the heart.
Venous Valves: Structure and Function
Venous valves are essentially folds of the tunica intima, the innermost layer of the venous wall. These folds are shaped like cusps or leaflets, which are typically paired. When blood flows towards the heart, the valve cusps open, allowing unimpeded flow. However, when blood attempts to flow backward, the cusps close, effectively sealing the vessel and preventing backflow. This action is entirely passive, relying on the pressure differences within the vein.
The precise structure of venous valves varies depending on their location and the size of the vein. Smaller veins may have only a single pair of cusps, while larger veins might have multiple cusps. The cusps are supported by a network of collagen and elastic fibers, which provide structural integrity and ensure the valve's proper function.
Key features of venous valves:
- Passive mechanism: They operate passively, relying on blood pressure gradients.
- Unidirectional flow: They permit blood flow in only one direction – towards the heart.
- Pressure-dependent: Their opening and closing are regulated by the pressure difference between the upstream and downstream segments of the vein.
- Varied structure: Their complexity varies depending on vessel size and location.
Locations of Venous Valves: A Detailed Exploration
Venous valves are not uniformly distributed throughout the venous system. Their distribution is strategically determined by the gravitational forces acting on the blood column. Valves are most abundant in veins of the lower extremities (legs and feet), where the effects of gravity are most pronounced. This dense concentration of valves helps counteract the force of gravity, promoting efficient venous return. The number of valves decreases progressively as we move towards the heart.
High density of venous valves in:
- Lower extremities: Legs, feet, and ankles have a high concentration of valves.
- Superficial veins: These veins closer to the skin surface have more valves than deep veins.
Lower density or absence of valves in:
- Large veins near the heart: Superior and inferior vena cavae typically lack valves.
- Some intracranial veins: Certain veins within the skull may have reduced or absent valves.
The precise location and number of valves are highly variable between individuals, reflecting the inherent plasticity of the circulatory system. This variability highlights the complexity of the venous system and the remarkable adaptability of its components.
Lymphatic Valves: Guardians of Lymphatic Flow
The lymphatic system, a crucial part of the immune system, plays a critical role in fluid balance and immune surveillance. Unlike the circulatory system, the lymphatic system doesn't have a central pump. Instead, it relies on a combination of factors, including smooth muscle contractions, skeletal muscle pump, and most importantly, lymphatic valves, to propel lymph unidirectionally towards the lymphatic ducts.
Lymphatic valves, similar in principle to venous valves, are unidirectional structures that prevent backflow of lymph. They are found throughout the lymphatic network, from the smallest lymphatic capillaries to larger lymphatic vessels. Their structure is similar to venous valves, consisting of folds of the intima lining the lymphatic vessel. However, lymphatic valves are often described as being more delicate and thinner than their venous counterparts.
The lymphatic system's reliance on valves is even more critical than the venous system due to the lack of a central pump. These valves ensure the continuous unidirectional flow of lymph, preventing stagnation and promoting efficient drainage of interstitial fluid. Stagnant lymph can lead to lymphedema, a condition characterized by fluid accumulation in the tissues.
Clinical Significance: Conditions Affecting Valved Vessels
Malfunction of venous or lymphatic valves can lead to a range of significant clinical conditions. These conditions often arise from a combination of factors, including genetic predisposition, aging, and lifestyle factors such as prolonged standing or sitting.
Venous insufficiency: A common ailment
Venous insufficiency, a prevalent condition, arises from the incompetence or failure of venous valves. This failure allows blood to flow backward, pooling in the veins and causing various symptoms, including:
- Varicose veins: These are visibly dilated and tortuous veins, often appearing as bulging, rope-like structures under the skin.
- Leg swelling (edema): Fluid accumulates in the tissues due to impaired venous return.
- Leg pain and cramps: These are often exacerbated by prolonged standing or physical activity.
- Skin changes: Chronic venous insufficiency can lead to discoloration and skin ulceration.
- Deep vein thrombosis (DVT): Although not directly caused by valve malfunction, venous insufficiency increases the risk of DVT.
Lymphedema: Impeded lymphatic drainage
Lymphedema, characterized by swelling due to impaired lymphatic drainage, can be primary (congenital) or secondary (acquired). Primary lymphedema arises from developmental abnormalities in the lymphatic system, while secondary lymphedema is often associated with conditions like cancer treatment, surgery, or infections that damage the lymphatic vessels or nodes.
Symptoms of lymphedema:
- Swelling: Often localized to a specific limb or region.
- Heaviness and discomfort: The affected limb feels heavy and uncomfortable.
- Limited range of motion: Swelling can restrict movement.
- Skin changes: The skin may become thickened and fibrotic.
- Increased risk of infection: Lymphedema can increase the risk of cellulitis.
Diagnostic Techniques for Valvular Disorders
Several diagnostic techniques are employed to assess the function of venous and lymphatic valves. These techniques aid in diagnosis and guide treatment strategies.
- Doppler ultrasound: This non-invasive technique uses sound waves to assess blood flow within the veins, allowing for the identification of incompetent valves and venous reflux.
- Venography: A more invasive technique involving the injection of contrast dye into the veins, providing detailed images of the venous system.
- Lymphoscintigraphy: This nuclear medicine technique uses radioactive tracers to visualize the lymphatic system, allowing for the assessment of lymphatic drainage and identification of obstructions.
- MRI and CT scans: These advanced imaging techniques can provide detailed anatomical information about the venous and lymphatic systems.
Treatment Options for Valvular Disorders
Treatment for valvular disorders depends on the severity of the condition and the individual's overall health. Treatment options may include:
- Conservative measures: These include lifestyle modifications like elevating the legs, wearing compression stockings, and regular exercise.
- Pharmacological therapies: Certain medications may be prescribed to reduce swelling and pain.
- Surgical interventions: In cases of severe venous insufficiency, surgical procedures such as vein stripping or ablation may be necessary. Lymphedema management often involves complex decongestive physiotherapy.
Conclusion: The Unsung Heroes of Circulation
The valves within our venous and lymphatic vessels are often overlooked, yet they play a crucial role in maintaining the efficient and unidirectional flow of blood and lymph. These unassuming structures work tirelessly to counteract gravity, prevent backflow, and ensure the proper functioning of our circulatory and lymphatic systems. Understanding their anatomy, physiology, and clinical significance is vital for the diagnosis and management of various circulatory disorders. By appreciating the significance of these valved vessels, we gain a deeper understanding of the intricate mechanisms that sustain our health and well-being. Further research into the intricate workings of these valves and the development of innovative treatments for related conditions continues to be a crucial area of focus in medical science.
Latest Posts
Latest Posts
-
Why Is Blood Classified As Connective Tissue
Mar 25, 2025
-
How Many Moles In 25 Grams Of Water
Mar 25, 2025
-
Energy Flow In An Ecosystem Begins With
Mar 25, 2025
-
How Many Moles Of Water Are In 1 Liter
Mar 25, 2025
-
Which One Of The Following Is Not A Strong Electrolyte
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Vessels That Contain Valves To Prevent Backflow Of Blood . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
