The Serous Membranes That Cover The Lungs Are Called The
News Leon
Mar 18, 2025 · 6 min read
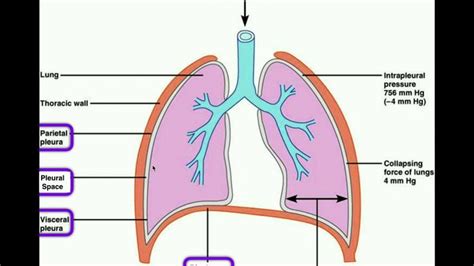
Table of Contents
The Serous Membranes That Cover the Lungs Are Called the Pleurae: A Deep Dive into Pulmonary Anatomy and Physiology
The lungs, the vital organs responsible for gas exchange, are not simply floating freely within the thoracic cavity. Instead, they are enveloped by a delicate yet crucial structure: the pleurae. Understanding the pleurae – their anatomy, their function, and their clinical significance – is paramount to comprehending respiratory health and disease. This article delves into the intricacies of the pleural membranes, exploring their structure, the fluid dynamics within the pleural space, and the implications of pleural pathologies.
The Anatomy of the Pleurae: A Double-Layered Protection
The pleura is a serous membrane, a thin, double-layered sac that completely encases each lung. Think of it as a deflated balloon carefully wrapped around the lung. This double-layered structure consists of two distinct parts:
1. Visceral Pleura: The Lung's Intimate Embrace
The visceral pleura is the inner layer, intimately adhering to the lung's surface. It follows every contour of the lung, including the fissures that divide the lobes. The visceral pleura is essentially part of the lung itself, and its smooth surface facilitates frictionless lung movement during respiration. It's richly supplied with blood vessels and nerve fibers, contributing to its sensitivity.
2. Parietal Pleura: The Thoracic Cavity's Lining
The parietal pleura is the outer layer, lining the thoracic cavity. It adheres to the inner surface of the chest wall, the diaphragm, the mediastinum (the space between the lungs containing the heart and other structures), and the superior surface of the diaphragm. Unlike the visceral pleura, the parietal pleura's innervation provides it with significant sensitivity, explaining the sharp pain associated with pleural inflammation. It is divided into several parts:
- Costal pleura: Covers the inner surface of the ribs and intercostal muscles.
- Diaphragmatic pleura: Covers the superior surface of the diaphragm.
- Mediastinal pleura: Lines the mediastinum.
- Cervical pleura (or cupola): Extends superiorly into the neck, reaching the level of the first rib.
The Pleural Space: A Potential Space with Vital Functions
Between the visceral and parietal pleurae lies the pleural space, also known as the pleural cavity. While referred to as a "space," it's actually a potential space, typically containing only a small amount (2-5 mL) of pleural fluid. This fluid acts as a crucial lubricant, minimizing friction between the two pleural layers during respiratory movements. The incredibly low pressure within the pleural space (-4 to -6 cm H₂O) helps maintain lung inflation and prevents lung collapse.
The Mechanics of Respiration: The Pleura's Crucial Role
The pleurae play a pivotal role in the mechanics of breathing. Their interplay ensures efficient gas exchange by facilitating lung expansion and recoil. Consider the following:
-
Inhalation: During inspiration, the diaphragm contracts and flattens, and the external intercostal muscles elevate the ribs. This increases the volume of the thoracic cavity, which, in turn, reduces the pressure within the pleural space. This negative pressure difference draws air into the lungs, expanding them. The visceral pleura is pulled along with the expanding lungs due to the surface tension of the pleural fluid, ensuring that the lungs follow the movements of the chest wall.
-
Exhalation: During expiration, the diaphragm relaxes and rises, and the intercostal muscles relax. This decreases the volume of the thoracic cavity, increasing the pressure in the pleural space. The elasticity of the lungs causes them to recoil, expelling air. The visceral pleura follows the lungs during this process.
Clinical Significance of Pleural Pathology: When Things Go Wrong
Several conditions can affect the pleura, leading to a range of symptoms and complications. Some key conditions include:
1. Pleuritis (Pleurisy): Inflammation of the Pleura
Pleuritis, also known as pleurisy, is inflammation of the pleura. This condition is often caused by infection (e.g., pneumonia, tuberculosis), autoimmune diseases, or cancer. The inflammation leads to pain, often described as a sharp, stabbing pain that worsens with deep breaths or coughing. A pleural friction rub – a grating sound heard during auscultation – is a characteristic finding.
2. Pleural Effusion: Fluid Accumulation in the Pleural Space
Pleural effusion refers to the abnormal accumulation of fluid in the pleural space. This can be caused by various factors, including heart failure (causing cardiogenic effusion), liver disease (causing transudative effusion), infections (causing exudative effusion), cancer (causing malignant effusion), and pulmonary embolism. The presence of excess fluid can compromise lung expansion and gas exchange, leading to shortness of breath. Thoracentesis (removal of fluid using a needle) is often necessary for diagnosis and treatment.
3. Pneumothorax: Air in the Pleural Space
Pneumothorax is the presence of air in the pleural space. This can occur spontaneously (spontaneous pneumothorax), due to trauma (traumatic pneumothorax), or as a complication of lung diseases (e.g., emphysema). The air in the pleural space disrupts the negative pressure, causing partial or complete lung collapse. Symptoms range from mild shortness of breath to severe respiratory distress, requiring medical intervention such as chest tube insertion to re-establish negative pressure.
4. Pleural Mesothelioma: A Rare and Aggressive Cancer
Pleural mesothelioma is a rare and aggressive cancer arising from the lining of the pleura. It is strongly associated with asbestos exposure. The prognosis is generally poor, although treatment options, including surgery, chemotherapy, and radiation therapy, are available. Early detection is crucial for improved outcomes.
Diagnostic Techniques for Pleural Diseases
Diagnosing pleural diseases often involves a combination of techniques, including:
- Chest X-ray: A common initial imaging technique to visualize the lungs and pleural space, identifying fluid accumulation, pneumothorax, or masses.
- Computed tomography (CT) scan: Provides more detailed images than chest X-rays, helping to characterize pleural lesions and identify underlying causes.
- Thoracentesis: The removal of pleural fluid using a needle, allowing for analysis of the fluid to determine its characteristics (e.g., exudative vs. transudative) and identify the underlying cause.
- Pleural biopsy: A procedure involving the removal of a tissue sample from the pleura for microscopic examination to diagnose conditions like cancer or infections.
Conclusion: The Pleurae – Silent Guardians of Respiratory Health
The pleurae are often overlooked, yet their crucial role in respiratory physiology is undeniable. Their delicate yet robust structure ensures frictionless lung movement, contributing to efficient gas exchange. Understanding the anatomy and physiology of the pleurae is fundamental to recognizing and managing pleural pathologies, which can have significant consequences for respiratory health. Early diagnosis and appropriate treatment are crucial for improving outcomes and maintaining quality of life for patients affected by pleural diseases. Further research continues to unravel the complexities of the pleurae and their role in both health and disease, paving the way for improved diagnostic and therapeutic approaches.
Latest Posts
Latest Posts
-
The Study Of Population Is Called
Mar 19, 2025
-
Oxidation Number Of O In H2o
Mar 19, 2025
-
Largest Cell Of The Human Body
Mar 19, 2025
-
Sin X Cos X 2 1 Sin 2x
Mar 19, 2025
-
Find The Surface Area Of The Square Pyramid Shown Below
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about The Serous Membranes That Cover The Lungs Are Called The . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
