The Juxtaglomerular Apparatus Is Composed Of ________.
News Leon
Mar 22, 2025 · 5 min read
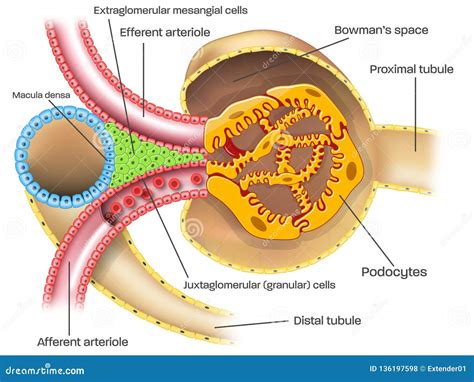
Table of Contents
The Juxtaglomerular Apparatus is Composed of: A Deep Dive into Renal Physiology
The juxtaglomerular apparatus (JGA) is a fascinating and crucial structure within the nephron, the functional unit of the kidney. Understanding its composition and function is key to comprehending how our bodies regulate blood pressure and electrolyte balance. This article will provide a comprehensive overview of the JGA, exploring its constituent parts in detail and explaining their roles in maintaining homeostasis.
The Components of the Juxtaglomerular Apparatus
The JGA is a specialized structure situated where the distal convoluted tubule (DCT) comes into close contact with the afferent and efferent arterioles of the glomerulus. It's a complex interplay of cells working in concert. Its key components include:
1. Granular Cells (Juxtaglomerular Cells):
- Location: These modified smooth muscle cells are located within the walls of the afferent arteriole, and to a lesser extent, the efferent arteriole. Their strategic placement is vital for their function.
- Function: Granular cells are the primary source of renin, a crucial enzyme in the renin-angiotensin-aldosterone system (RAAS). Renin plays a pivotal role in regulating blood pressure by initiating a cascade that ultimately leads to increased sodium and water retention. The release of renin is triggered by various stimuli, including decreased blood pressure, decreased sodium concentration in the distal tubule, and sympathetic nervous system activation. This intricate mechanism ensures appropriate responses to changes in the body's internal environment. They also produce erythropoietin in smaller amounts.
2. Macula Densa:
- Location: This specialized group of epithelial cells is found in the distal convoluted tubule (DCT) at the point where it contacts the afferent arteriole. The cells are tightly packed, giving them a distinct appearance under a microscope.
- Function: The macula densa acts as a sodium sensor. It detects changes in the concentration of sodium chloride (NaCl) in the fluid flowing through the DCT. A decrease in NaCl concentration signals a decrease in glomerular filtration rate (GFR). This triggers the macula densa to signal the granular cells to release renin. This feedback loop is critical for maintaining a stable GFR and blood pressure. They also play a role in tubuloglomerular feedback, which fine-tunes GFR in response to changes in distal tubular flow.
3. Extraglomerular Mesangial Cells (Lacis Cells):
- Location: These cells are situated between the afferent and efferent arterioles and the macula densa. They form a supportive network connecting the other components of the JGA.
- Function: While their precise role is still being researched, extraglomerular mesangial cells are believed to have a paracrine function, communicating with both the granular cells and macula densa. They are thought to play a role in regulating renin release and GFR. They may also contribute to the structural integrity of the JGA and modulate its response to various stimuli. Their interconnection with the other cells suggests a role in coordinating the overall response of the JGA.
The Renin-Angiotensin-Aldosterone System (RAAS) and its Relation to the JGA
The JGA's primary function is inextricably linked to the RAAS, a hormonal system that regulates blood volume and blood pressure. The process begins with the release of renin from the granular cells of the JGA.
-
Renin Release: As previously mentioned, various stimuli trigger renin release, including low blood pressure, low sodium concentration in the DCT, and sympathetic stimulation.
-
Angiotensinogen Conversion: Renin acts on angiotensinogen, a protein produced by the liver, converting it to angiotensin I.
-
Angiotensin-Converting Enzyme (ACE): Angiotensin I is then converted to angiotensin II by ACE, an enzyme primarily found in the lungs.
-
Angiotensin II Effects: Angiotensin II is a potent vasoconstrictor, causing blood vessels to narrow, increasing peripheral resistance, and thus elevating blood pressure. It also stimulates the adrenal cortex to release aldosterone.
-
Aldosterone Effects: Aldosterone acts on the distal tubules and collecting ducts of the nephron, promoting sodium reabsorption and potassium excretion. This leads to increased water retention, further increasing blood volume and blood pressure.
Clinical Significance of the JGA
Dysfunction of the JGA can have significant clinical implications, often leading to conditions like:
- Hypertension: Overproduction of renin can lead to excessive activation of the RAAS, resulting in sustained high blood pressure.
- Hypotension: Underproduction of renin can cause low blood pressure due to inadequate activation of the RAAS.
- Renal Failure: Damage to the JGA can impair its ability to regulate blood pressure and electrolyte balance, potentially contributing to kidney failure.
- Certain types of kidney disease: Conditions affecting the kidneys can often disrupt the normal functioning of the JGA, which may further exacerbate the disease progression.
Further Research and Understanding
The JGA remains an area of active research. Scientists continue to investigate the precise mechanisms involved in renin release and the complex interactions between the various cell types within the apparatus. A deeper understanding of these processes holds promise for the development of more effective treatments for hypertension and other related conditions. Specific research areas include clarifying the role of extraglomerular mesangial cells, further investigating the intricate signaling pathways involved in tubuloglomerular feedback, and exploring the potential for targeted therapies that modulate JGA activity.
Conclusion
The juxtaglomerular apparatus is a remarkably intricate and vital structure within the kidney. Its composition—granular cells, macula densa, and extraglomerular mesangial cells—works in harmony to regulate blood pressure and electrolyte balance via the renin-angiotensin-aldosterone system. A thorough understanding of the JGA is crucial for comprehending normal renal physiology and the pathophysiology of several important clinical conditions. As research continues, we can expect even greater insight into this fascinating component of the renal system and its profound impact on overall health. Further studies will undoubtedly reveal more details about its complex interactions and contribute to advancements in the treatment of various kidney-related diseases. The JGA's role in maintaining homeostasis underlines its importance in the body's overall well-being. Its intricate mechanisms and profound physiological impact highlight the complexity and efficiency of the human body's regulatory systems.
Latest Posts
Latest Posts
-
Water Evaporating Physical Or Chemical Change
Mar 22, 2025
-
Which Type Of Leukocyte Releases Histamine
Mar 22, 2025
-
Blood Acquires Its Red Color From
Mar 22, 2025
-
The Working People Of France Were Called The
Mar 22, 2025
-
How Do You Balance C2h6 O2 Co2 H2o
Mar 22, 2025
Related Post
Thank you for visiting our website which covers about The Juxtaglomerular Apparatus Is Composed Of ________. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
