The Interstitial Cells Of The Testes Produce
News Leon
Mar 21, 2025 · 6 min read
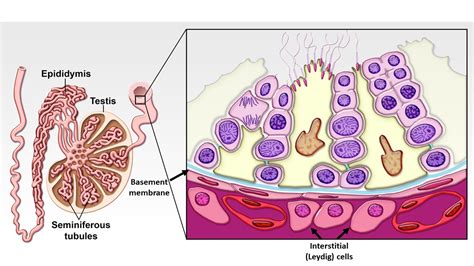
Table of Contents
The Interstitial Cells of the Testes: Producers of Testosterone and More
The interstitial cells of Leydig, also known as Leydig cells, are essential components of the testes, playing a pivotal role in male sexual development and reproductive function. These cells are located in the interstitial spaces between the seminiferous tubules, the structures responsible for sperm production. Their primary function is the production of testosterone, the primary male sex hormone, but their influence extends far beyond this crucial role. This article will delve into the intricate workings of Leydig cells, exploring their development, function, regulation, and clinical significance.
The Development of Leydig Cells: From Embryo to Adulthood
The journey of Leydig cells begins during fetal development. Fetal Leydig cells emerge early in gestation, contributing to the masculinization of the male fetus. They are crucial for the development of the Wolffian ducts, which differentiate into the epididymis, vas deferens, and seminal vesicles. These fetal Leydig cells are characterized by their transient nature; their numbers peak during specific gestational periods before gradually declining.
Following a period of quiescence after birth, adult Leydig cells begin to develop during puberty, triggered by the surge of luteinizing hormone (LH) from the anterior pituitary gland. These adult cells are responsible for the sustained production of testosterone throughout adulthood, maintaining secondary sexual characteristics and supporting spermatogenesis. Adult Leydig cells differ from their fetal counterparts in terms of size, morphology, and steroidogenic capacity.
The Production of Testosterone: A Complex Endocrine Process
The cornerstone of Leydig cell function is the biosynthesis of testosterone. This intricate process involves a series of enzymatic reactions, primarily within the mitochondria and smooth endoplasmic reticulum of the cell. The process begins with cholesterol, which is transported into the Leydig cells via low-density lipoproteins (LDLs).
Here's a simplified breakdown of the testosterone synthesis pathway:
-
Cholesterol uptake and transport: Cholesterol enters the Leydig cell via LDL receptors.
-
Cholesterol esterification and storage: Cholesterol is esterified and stored in lipid droplets.
-
Cholesterol transport to the mitochondria: Cholesterol is transported to the inner mitochondrial membrane, where the rate-limiting step in steroidogenesis occurs.
-
Side-chain cleavage: The cholesterol side chain is cleaved by the cytochrome P450 enzyme, CYP11A1, forming pregnenolone.
-
Pregnenolone conversion: Pregnenolone undergoes a series of enzymatic conversions, including 3β-hydroxysteroid dehydrogenase (3β-HSD), 17α-hydroxylase (CYP17A1), and 17,20-lyase (CYP17A1), ultimately leading to the formation of androstenedione.
-
Androstenedione conversion: Androstenedione is converted to testosterone by 17β-hydroxysteroid dehydrogenase (17β-HSD).
-
Testosterone secretion: Testosterone is secreted into the bloodstream, bound to sex hormone-binding globulin (SHBG) and albumin.
This meticulous process is highly regulated, ensuring the appropriate levels of testosterone are produced to meet the body's needs.
Regulation of Testosterone Production: A Delicate Balance
The production of testosterone is under tight hormonal control, primarily involving the hypothalamic-pituitary-gonadal (HPG) axis. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
-
LH: The principal regulator of testosterone production. LH binds to its receptor on Leydig cells, activating the intracellular signaling pathways that ultimately lead to increased testosterone synthesis.
-
FSH: While primarily involved in spermatogenesis, FSH also plays a modulatory role in Leydig cell function. It can influence the expression of steroidogenic enzymes and the sensitivity of Leydig cells to LH.
Other factors influencing testosterone production include:
-
Local paracrine factors: Several factors produced within the testes, such as growth factors and cytokines, can modulate Leydig cell function.
-
Systemic factors: Factors such as nutritional status, stress, and certain medications can impact testosterone production.
This complex interplay of hormonal and local factors ensures that testosterone levels are maintained within a physiological range, crucial for maintaining reproductive health and overall well-being.
Beyond Testosterone: Other Functions of Leydig Cells
While testosterone production is the most prominent function, evidence suggests that Leydig cells may contribute to other aspects of male reproductive health.
-
Growth Factors and Cytokines: Leydig cells produce various growth factors and cytokines that may influence the development and function of surrounding cells within the testes, including Sertoli cells and germ cells.
-
Immune Regulation: Leydig cells express various immune-related molecules, suggesting a potential role in regulating the immune response within the testes, creating an immunoprivileged environment for sperm development.
-
Extra-gonadal functions: Recent research suggests Leydig cells might have extra-gonadal effects, influencing other physiological processes such as bone metabolism, cardiovascular function, and cognitive function, although these roles are still under investigation.
Clinical Significance: Disorders Affecting Leydig Cell Function
Disruptions in Leydig cell function can lead to several clinical conditions, affecting both sexual development and reproductive health.
-
Hypogonadism: A condition characterized by deficient testosterone production, resulting in various symptoms such as reduced libido, erectile dysfunction, infertility, and decreased muscle mass. Causes can range from genetic defects to acquired conditions like infections or trauma.
-
Leydig Cell Tumors: Benign or malignant tumors arising from Leydig cells can lead to hormonal imbalances, potentially causing precocious puberty in boys or gynecomastia (breast enlargement) in adult males.
-
Klinefelter Syndrome: A genetic condition characterized by an extra X chromosome (XXY) that often results in reduced Leydig cell function and hypogonadism.
-
Exposure to endocrine disruptors: Exposure to certain environmental chemicals, known as endocrine disruptors, can interfere with Leydig cell function and testosterone production.
Diagnosing and managing Leydig cell-related disorders requires careful evaluation of hormonal levels, imaging studies, and potentially genetic testing. Treatment strategies may involve hormone replacement therapy, surgery, or management of underlying conditions.
Future Directions: Ongoing Research and Unanswered Questions
Despite significant advancements in our understanding of Leydig cells, several aspects of their biology remain to be elucidated. Ongoing research focuses on:
-
Detailed mechanisms of testosterone regulation: Further investigation is needed to fully understand the complex interplay of factors regulating testosterone production at the molecular and cellular levels.
-
Paracrine and autocrine functions: The complete range of local factors produced by Leydig cells and their influence on neighboring cells requires further exploration.
-
Extra-gonadal effects of Leydig cells: Investigating the potential systemic impacts of Leydig cells beyond their role in reproductive function could reveal new therapeutic targets for various diseases.
-
Leydig cell dysfunction in age-related diseases: The role of Leydig cell dysfunction in conditions such as age-related decline in testosterone, cardiovascular disease, and osteoporosis, warrants further study.
Conclusion
The interstitial cells of Leydig are far more than simple testosterone factories. These essential cells play a multifaceted role in male reproductive health and potentially influence other physiological processes. A deeper understanding of their development, function, and regulation is crucial for improving the diagnosis and management of disorders affecting Leydig cell function and advancing our knowledge of male reproductive biology. Continuous research in this area will undoubtedly reveal further insights into the intricate workings of these remarkable cells and their vital contribution to male health.
Latest Posts
Latest Posts
-
Seven More Than Twice A Number Is Equal To 25
Mar 28, 2025
-
The Part Of Earth Where Life Exists
Mar 28, 2025
-
What Intermolecular Forces Are Present In Ch4
Mar 28, 2025
-
A Man Was Murdered In His Office Riddle
Mar 28, 2025
-
A Coil Is Formed By Winding 250 Turns
Mar 28, 2025
Related Post
Thank you for visiting our website which covers about The Interstitial Cells Of The Testes Produce . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
