Correctly Label The Following Parts Of The Testis.
News Leon
Mar 28, 2025 · 6 min read
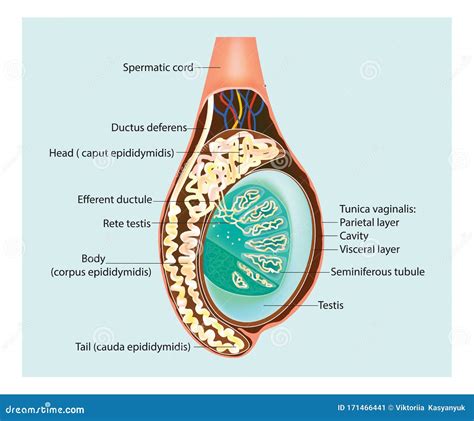
Table of Contents
Correctly Label the Following Parts of the Testis: A Comprehensive Guide
The testes, or testicles, are the male gonads responsible for producing sperm and testosterone. Understanding their intricate anatomy is crucial for anyone studying human biology, medicine, or related fields. This comprehensive guide will delve into the detailed structure of the testis, enabling you to correctly label its various components. We'll explore each part, its function, and its significance in male reproductive health.
The External Anatomy of the Testis
Before diving into the internal structures, let's examine the external features visible to the naked eye. The testis is an ovoid structure, typically around 4-5 cm in length and 2-3 cm in diameter. Its external anatomy includes:
1. Tunica Albuginea:
This is the tough, fibrous, white capsule that encloses the testis. It's a critical protective layer, providing structural support and safeguarding the delicate internal tissues. The tunica albuginea is responsible for maintaining the testis's shape and integrity. Its thickness and density vary across the surface.
2. Tunica Vaginalis:
This is a serous membrane derived from the peritoneum. It forms a double-layered sac that partially surrounds the testis and epididymis. The visceral layer is intimately attached to the testis, while the parietal layer lines the scrotal cavity. The space between these two layers contains a small amount of serous fluid, allowing for frictionless movement within the scrotum. Inflammation of the tunica vaginalis is known as hydrocele.
3. Mediastinum Testis:
This is a thickening of the tunica albuginea located on the posterior aspect of the testis. It's a crucial landmark as it serves as the entry point for the testicular vessels and efferent ductules. The mediastinum testis is pivotal in supporting the internal structure of the organ and facilitating the transport of fluids.
The Internal Anatomy of the Testis: Delving into the Seminiferous Tubules
The interior of the testis is dominated by a complex network of tightly packed seminiferous tubules. These are the sites of sperm production, a process known as spermatogenesis. Let's explore the key internal components:
1. Seminiferous Tubules:
These are highly convoluted tubes that form the bulk of the testicular parenchyma. Their highly folded structure dramatically increases the surface area available for sperm production. The seminiferous tubules are lined with specialized cells:
-
Sertoli cells: These are nurse cells that support and nourish developing sperm cells. They provide essential nutrients, regulate spermatogenesis, and create a protective environment for the delicate germ cells. Sertoli cells also play a vital role in the blood-testis barrier, preventing immune system attack on developing sperm.
-
Germ cells: These are the precursor cells that undergo meiosis to produce sperm. The process involves several stages, from spermatogonia (stem cells) to spermatocytes (undergoing meiosis) to spermatids (haploid cells) and finally spermatozoa (mature sperm).
2. Leydig Cells (Interstitial Cells):
These are endocrine cells located in the interstitial tissue between the seminiferous tubules. Leydig cells are responsible for the production of testosterone, the primary male sex hormone. Testosterone is essential for the development of secondary sexual characteristics, spermatogenesis, and maintaining libido.
3. Rete Testis:
This is a network of interconnected tubules located within the mediastinum testis. The rete testis receives sperm from the seminiferous tubules and transports them to the efferent ductules. It acts as a crucial transit point in the journey of sperm from production to storage.
4. Efferent Ductules:
These are small ducts that carry sperm from the rete testis to the epididymis. They are characterized by their unique structure, featuring both ciliated and non-ciliated cells. The cilia help move sperm towards the epididymis, while the non-ciliated cells aid in fluid absorption.
Beyond the Testis: Connecting to the Male Reproductive System
The testis is not an isolated organ; its function is intricately linked to the rest of the male reproductive system. Understanding these connections is crucial for a complete picture.
1. Epididymis:
This is a highly coiled tube located on the posterior surface of the testis. The efferent ductules deliver sperm to the epididymis, where they undergo maturation and storage. The epididymis plays a vital role in sperm capacitation, a process that makes sperm fully fertile. It's divided into three parts: the head (caput), body (corpus), and tail (cauda).
2. Vas Deferens (Ductus Deferens):
This is a muscular tube that transports mature sperm from the epididymis to the ejaculatory ducts. Its strong muscular contractions propel sperm forward during ejaculation. The vas deferens is part of the spermatic cord, along with blood vessels, nerves, and lymphatics. Vasectomy, a form of male sterilization, involves severing the vas deferens.
3. Spermatic Cord:
This structure is a bundle of tissues that suspends the testis within the scrotum. It includes the vas deferens, testicular arteries and veins, nerves, and lymphatic vessels. The spermatic cord provides the necessary vascular supply and neural connections for testicular function. It also plays a role in thermoregulation, keeping the testes at a slightly lower temperature than core body temperature.
4. Blood Supply:
The testes receive their blood supply from the testicular arteries, branches of the abdominal aorta. These arteries provide oxygen and nutrients essential for spermatogenesis and testosterone production. Venous drainage occurs via the pampiniform plexus, a network of veins that surrounds the testicular artery. The pampiniform plexus plays a critical role in thermoregulation by countercurrent heat exchange.
5. Lymphatic Drainage:
Lymphatic vessels drain lymph from the testis to the para-aortic lymph nodes, located in the abdomen. This drainage system is crucial for the removal of waste products and the maintenance of immune surveillance.
Clinical Significance: Understanding Testicular Disorders
Knowledge of the testicular anatomy is essential for understanding various clinical conditions affecting the male reproductive system. Several diseases and disorders can affect the testis, impacting its ability to produce sperm and testosterone. These include:
-
Testicular Cancer: This is a relatively rare but potentially life-threatening cancer that originates in the germ cells or Leydig cells of the testis. Early detection and treatment are crucial for improving prognosis.
-
Varicocele: This is the abnormal enlargement of the veins within the pampiniform plexus. It can lead to impaired testicular function due to reduced blood flow and increased temperature.
-
Hydrocele: This is the accumulation of fluid within the tunica vaginalis, resulting in swelling of the scrotum. Hydroceles can be caused by inflammation or obstruction of lymphatic drainage.
-
Orchitis: This is inflammation of the testis, often caused by infection, such as mumps. Orchitis can lead to impaired testicular function and potential sterility.
-
Cryptorchidism: This condition involves the failure of one or both testes to descend into the scrotum during fetal development. Cryptorchidism increases the risk of testicular cancer and infertility.
Conclusion: Mastering the Anatomy of the Testis
This comprehensive guide has provided a detailed exploration of the testis, from its external features to its intricate internal structures and connections within the male reproductive system. Understanding the anatomy of the testis is crucial for appreciating its vital role in male reproductive health, diagnosing various disorders, and developing effective treatment strategies. By grasping the details of the tunica albuginea, seminiferous tubules, Leydig cells, rete testis, efferent ductules, epididymis, vas deferens, and the surrounding vascular and lymphatic systems, you build a strong foundation in male reproductive biology. Remember that this information is for educational purposes and should not be considered medical advice. Always consult with a healthcare professional for any health concerns.
Latest Posts
Latest Posts
-
How Many Hydrogen Bonds Between C And G
Mar 29, 2025
-
Regulates What Enters And Leaves The Cell
Mar 29, 2025
-
The Most Active Phagocytic Cells In Circulating Blood Are
Mar 29, 2025
-
How Many Cups In 9 Ounces
Mar 29, 2025
-
How Many Ones Are There Between 1 And 100
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Correctly Label The Following Parts Of The Testis. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
