What Is Not True About Antibodies
News Leon
Apr 07, 2025 · 7 min read
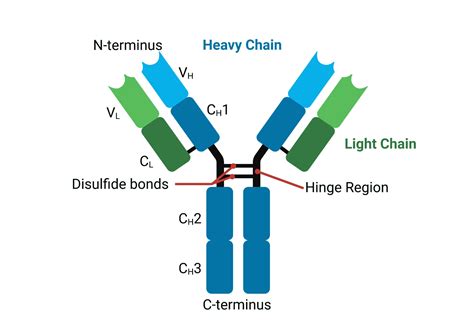
Table of Contents
What's Not True About Antibodies: Debunking Common Myths
Antibodies, also known as immunoglobulins (Ig), are glycoprotein molecules produced by plasma cells (white blood cells). They are crucial components of the adaptive immune system, playing a vital role in defending the body against pathogens like bacteria, viruses, fungi, and parasites. While their function is generally well-understood, several misconceptions surrounding antibodies persist. This article aims to debunk some common myths and clarify the realities of antibody function and behavior.
Myth 1: Antibodies Directly Kill Pathogens
Reality: Antibodies don't directly kill pathogens in most cases. Instead, they act as highly specific "targeting systems," marking pathogens for destruction by other components of the immune system. This process involves several mechanisms:
Neutralization:
Antibodies bind to specific sites on pathogens, such as viral surface proteins or bacterial toxins. This binding physically blocks the pathogen's ability to infect host cells or exert its harmful effects. Think of it like covering a keyhole with glue, preventing the "key" (pathogen) from entering the "door" (host cell).
Opsonization:
Antibodies coat the surface of pathogens, making them more easily recognized and engulfed by phagocytic cells (like macrophages and neutrophils). These phagocytes have receptors that specifically bind to antibodies, enhancing the efficiency of pathogen destruction. This is like adding a "handle" to the pathogen, making it easier for the phagocytes to grab and eliminate.
Complement Activation:
The binding of antibodies to pathogens can trigger the complement system, a cascade of protein reactions that leads to pathogen lysis (destruction), inflammation, and enhanced phagocytosis. It's like calling in reinforcements – a powerful army of proteins that further attack and eliminate the threat.
Antibody-Dependent Cell-mediated Cytotoxicity (ADCC):
Certain immune cells, like natural killer (NK) cells, possess receptors that bind to antibodies attached to infected cells. This binding triggers the NK cells to release cytotoxic granules, killing the infected cells. This is like using guided missiles to target and destroy infected cells.
Myth 2: All Antibodies are Created Equal
Reality: The immune system produces a vast repertoire of antibodies, each with unique specificity for a particular antigen (a molecule that triggers an immune response). These antibodies are categorized into five main classes or isotypes: IgA, IgD, IgE, IgG, and IgM. Each isotype has distinct structural features and functions:
-
IgG: The most abundant antibody in the blood, playing a crucial role in opsonization, complement activation, and ADCC. It's also the only antibody that can cross the placenta, providing passive immunity to the fetus.
-
IgM: The first antibody produced during an immune response, playing a significant role in complement activation. It's also effective in agglutination (clumping together) of pathogens.
-
IgA: Found primarily in mucosal secretions (tears, saliva, breast milk), it protects against pathogens entering the body through mucosal surfaces.
-
IgE: Involved in allergic reactions and defense against parasites. It binds to mast cells and basophils, triggering the release of histamine and other inflammatory mediators.
-
IgD: Its function is less well understood, but it's believed to play a role in B cell activation and development.
These differences in structure and function highlight the diversity and complexity of the antibody response. There's no single "best" antibody; each isotype is uniquely adapted to perform specific roles in different parts of the immune system.
Myth 3: Antibodies are Only Effective Against Infections
Reality: While antibodies play a crucial role in fighting infections, their functions extend beyond this. They are involved in a range of other biological processes:
-
Autoimmune diseases: In autoimmune diseases, the immune system mistakenly attacks the body's own tissues. This can involve the production of autoantibodies (antibodies that target self-antigens).
-
Cancer: Antibodies are being developed and used therapeutically in cancer treatment. These antibodies, often engineered to target specific cancer cells, can directly kill cancer cells or enhance the activity of the immune system against them.
-
Diagnostic tools: Antibodies are crucial components of numerous diagnostic tests, such as ELISA (enzyme-linked immunosorbent assay) and Western blot, used to detect the presence of specific antigens or antibodies in a sample. This allows for the detection of infections or other conditions.
-
Therapeutic agents: Antibodies are utilized in therapeutic applications, including the treatment of various inflammatory conditions and autoimmune diseases. They can neutralize harmful molecules or block specific signaling pathways involved in disease pathogenesis.
Myth 4: Antibody Production is a Quick Process
Reality: While the body can rapidly produce antibodies against some pathogens, the full antibody response typically takes several days to weeks to develop. This response involves a series of steps:
-
Antigen recognition: Immune cells, such as B cells, encounter and recognize the foreign antigen.
-
B cell activation: The antigen-specific B cells are activated and begin to proliferate (multiply).
-
Antibody production: The activated B cells differentiate into plasma cells, which are specialized antibody-producing cells.
-
Antibody maturation: The antibodies produced undergo a process of affinity maturation, resulting in antibodies with increased binding strength to the antigen.
-
Memory cell formation: Some activated B cells differentiate into memory B cells, which provide long-lasting immunity against future encounters with the same antigen.
This intricate process ensures that the immune response is effective and tailored to the specific pathogen. The time required for antibody production varies depending on factors such as the nature of the antigen and the individual's immune status.
Myth 5: Higher Antibody Levels Always Mean Better Protection
Reality: While higher antibody levels often correlate with better protection, this isn't always the case. The quality and functionality of the antibodies are just as important as their quantity. For example:
-
Antibody isotype: The type of antibody (IgG, IgM, etc.) influences its effectiveness. IgG is generally more effective than IgM in providing long-lasting immunity.
-
Antibody affinity: The strength of antibody binding to the antigen (affinity) is crucial for neutralizing the pathogen or triggering other immune effector functions. Higher affinity antibodies are generally more effective.
-
Antibody specificity: Antibodies must be highly specific for the target antigen to avoid cross-reactivity with other molecules. Non-specific antibody responses can be counterproductive and harmful.
Simply measuring the total antibody level doesn't provide a complete picture of the immune response. Sophisticated assays are required to assess the quality and functionality of antibodies to fully understand the level of protection provided.
Myth 6: Once You Have Antibodies, You're Immune For Life
Reality: While some infections result in life-long immunity (like measles), others require repeated boosting of the immune system through re-infection or vaccination. The durability of antibody-mediated immunity varies depending on several factors:
-
The nature of the pathogen: Some pathogens are more adept at evading the immune system than others. Viruses like influenza undergo frequent mutations, rendering previous antibody responses less effective.
-
The individual's immune status: The age and overall health of an individual influence the strength and longevity of their antibody response. Immunocompromised individuals may have weaker and shorter-lived antibody responses.
-
The type of immune response: The development of memory B cells plays a crucial role in long-lasting immunity. The more robust the memory B cell response, the longer the immunity will last.
Therefore, while antibodies provide a crucial layer of protection, they are not a guarantee of lifelong immunity against all pathogens. Regular booster shots for certain diseases are necessary to maintain optimal protection levels.
Conclusion
Antibodies are remarkable molecules that play a vital role in protecting the body against a wide range of threats. While their primary function is to mark pathogens for destruction rather than direct killing, their roles are multifaceted and extend beyond infection control. Understanding the complexities of antibody function and dispelling common myths is crucial for developing effective strategies for disease prevention and treatment. This comprehensive understanding necessitates moving beyond simple antibody level measurements and instead focusing on quality, specificity, and the interplay with other components of the immune system for a holistic view of immunity.
Latest Posts
Latest Posts
-
The Outer Covering Of Bone Is The
Apr 11, 2025
-
What Is 2 3 Of 42
Apr 11, 2025
-
Prokaryotic Cells Have A Nucleus True Or False
Apr 11, 2025
-
The Type Of Rock Shown In This Photograph Is
Apr 11, 2025
-
Which Of The Following Compounds Is Not An Enzyme
Apr 11, 2025
Related Post
Thank you for visiting our website which covers about What Is Not True About Antibodies . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.