Select The Correct Statement About Cardiac Output
News Leon
Mar 26, 2025 · 6 min read
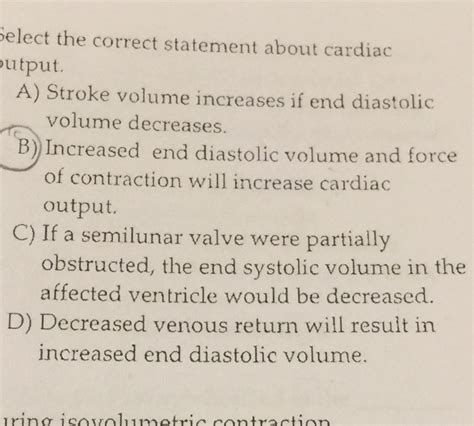
Table of Contents
- Select The Correct Statement About Cardiac Output
- Table of Contents
- Select the Correct Statement About Cardiac Output: A Deep Dive into Cardiovascular Physiology
- Understanding Cardiac Output: The Heart's Workload
- Heart Rate (HR): The Pace of the Pump
- Stroke Volume (SV): The Volume of Each Beat
- Factors Affecting Cardiac Output: A Complex Interplay
- Measuring Cardiac Output: Methods and Techniques
- Implications of Altered Cardiac Output: Clinical Significance
- Selecting the Correct Statement: Debunking Misconceptions
- Conclusion: A Dynamic and Essential Parameter
- Latest Posts
- Latest Posts
- Related Post
Select the Correct Statement About Cardiac Output: A Deep Dive into Cardiovascular Physiology
Cardiac output (CO), a cornerstone of cardiovascular physiology, represents the volume of blood pumped by the heart per minute. Understanding its intricacies is crucial for comprehending overall circulatory health and diagnosing various cardiovascular conditions. This article delves deep into the concept of cardiac output, exploring the factors that influence it, the methods used for its measurement, and the implications of its alterations. We'll also dissect common misconceptions and select the most accurate statement about cardiac output from a range of possibilities.
Understanding Cardiac Output: The Heart's Workload
Cardiac output is a product of two key variables: heart rate (HR) and stroke volume (SV). The formula is elegantly simple:
Cardiac Output (CO) = Heart Rate (HR) x Stroke Volume (SV)
Let's break down these components:
Heart Rate (HR): The Pace of the Pump
Heart rate, measured in beats per minute (bpm), dictates the frequency of ventricular contractions. It's influenced by the autonomic nervous system (ANS), hormones, and various other factors. The sympathetic nervous system accelerates HR, while the parasympathetic nervous system (via the vagus nerve) slows it down. Hormones like adrenaline and noradrenaline significantly increase HR, preparing the body for "fight or flight" responses. Electrolyte imbalances, particularly those involving potassium and calcium, can also impact HR.
Stroke Volume (SV): The Volume of Each Beat
Stroke volume, measured in milliliters (ml) or liters (L), represents the amount of blood ejected from the left ventricle with each contraction. Several factors influence SV:
-
Preload: This refers to the degree of ventricular stretch at the end of diastole (ventricular relaxation). Increased venous return leads to increased preload, enhancing the force of contraction (Frank-Starling mechanism). Conditions like dehydration can decrease preload, reducing SV.
-
Afterload: This represents the resistance the left ventricle encounters when ejecting blood into the aorta. Increased afterload (e.g., due to hypertension or aortic stenosis) reduces SV as the heart has to work harder to overcome the resistance.
-
Contractility: This reflects the inherent ability of the myocardium (heart muscle) to contract forcefully. Factors like sympathetic stimulation, certain medications (inotropes), and the availability of calcium ions impact contractility. Weakened myocardium (e.g., in heart failure) results in decreased contractility and reduced SV.
Factors Affecting Cardiac Output: A Complex Interplay
Numerous factors beyond HR and SV contribute to the overall cardiac output. These include:
-
Blood Volume: The total amount of blood in the circulatory system directly influences venous return and preload, subsequently affecting SV. Hypovolemia (low blood volume) diminishes CO, while hypervolemia can initially increase it, although excessive volume can strain the heart.
-
Blood Viscosity: Thicker blood (increased viscosity) increases afterload, making it more difficult for the heart to pump blood, thereby reducing CO. Conditions like polycythemia (increased red blood cell count) increase viscosity.
-
Peripheral Vascular Resistance (PVR): The overall resistance to blood flow in the peripheral blood vessels significantly impacts afterload. Vasoconstriction (narrowing of blood vessels) increases PVR, while vasodilation (widening of blood vessels) decreases it.
-
Body Temperature: Increased body temperature generally increases HR and contractility, enhancing CO. Conversely, decreased temperature slows HR and reduces contractility.
-
Age: Cardiac output typically decreases with age, primarily due to reduced cardiac contractility and increased stiffness of the heart muscle.
-
Physical Fitness: Regular exercise strengthens the heart muscle, increasing contractility and reducing resting HR, ultimately improving CO.
-
Hormonal Influences: Hormones such as thyroid hormones, adrenaline, and noradrenaline affect HR and contractility, impacting CO. Thyroid hormone excess (hyperthyroidism) can dramatically increase CO.
Measuring Cardiac Output: Methods and Techniques
Accurately measuring cardiac output is crucial in clinical settings. Various methods exist, each with its strengths and limitations:
-
Thermodilution (Swan-Ganz Catheter): This invasive technique involves injecting a cold bolus of saline into the pulmonary artery and measuring the temperature change as it mixes with the blood. The rate of temperature change is used to calculate CO.
-
Echocardiography: This non-invasive imaging technique uses ultrasound to visualize the heart and measure the dimensions of the heart chambers and the ejection fraction (EF), which is the percentage of blood ejected from the ventricle with each contraction. EF is a crucial indicator of SV and CO.
-
Doppler Ultrasound: Similar to echocardiography, Doppler ultrasound uses sound waves to measure blood flow velocity in various vessels. This information can be used to estimate CO.
-
Electrocardiography (ECG): While ECG primarily measures the electrical activity of the heart, it can indirectly provide clues about HR and, to some extent, the regularity of contractions, which can be useful in assessing CO.
-
Cardiac Magnetic Resonance Imaging (CMR): CMR is a non-invasive imaging technique offering detailed information about the heart's structure and function. It can be used to assess the ejection fraction and other parameters relevant to CO determination.
Implications of Altered Cardiac Output: Clinical Significance
Alterations in cardiac output have significant clinical implications, with both increased and decreased CO causing problems:
Low Cardiac Output (Hypovolemic Shock, Cardiogenic Shock): This signifies insufficient blood supply to meet the body's metabolic demands, leading to tissue hypoxia and organ damage. Causes include heart failure, severe dehydration, and massive blood loss.
High Cardiac Output (Hyperkinetic Circulation): While often associated with conditions like hyperthyroidism and pregnancy, excessive CO can strain the heart over time.
Selecting the Correct Statement: Debunking Misconceptions
Now, let's address the main question: selecting the correct statement about cardiac output. Consider these statements, with only one being entirely accurate:
- Statement A: Cardiac output is solely determined by heart rate.
- Statement B: Stroke volume is unaffected by preload and afterload.
- Statement C: Increased blood viscosity always increases cardiac output.
- Statement D: Cardiac output is the product of heart rate and stroke volume.
The correct statement is D. Cardiac output is indeed the product of heart rate and stroke volume, as the fundamental formula clearly illustrates. Statements A, B, and C are inaccurate because they misrepresent the complex interplay of factors that determine cardiac output.
Conclusion: A Dynamic and Essential Parameter
Cardiac output is a dynamic parameter reflecting the heart's effectiveness in pumping blood. It's influenced by a multitude of intricate factors, highlighting the interconnectedness of cardiovascular function. Understanding these factors and the methods used to measure CO is essential for diagnosing, managing, and treating various cardiovascular conditions. This comprehensive exploration aims to equip readers with a deeper understanding of this fundamental concept in physiology. Further research and continuous learning remain crucial to grasping the complexities of this critical aspect of human health. The information provided here is for educational purposes only and should not be considered medical advice. Consult a qualified healthcare professional for any health concerns.
Latest Posts
Latest Posts
-
A Fully Loaded Slow Moving Freight Elevator
Mar 30, 2025
-
62 Rounded To The Nearest Ten
Mar 30, 2025
-
The Longest Side Of A Right Triangle Is Called The
Mar 30, 2025
-
Which Of The Following Is True Of Mitosis
Mar 30, 2025
-
Which Of The Following Is A Variable Cost
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about Select The Correct Statement About Cardiac Output . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
