Red And White Blood Cells In Fluid Matrix
News Leon
Mar 18, 2025 · 6 min read
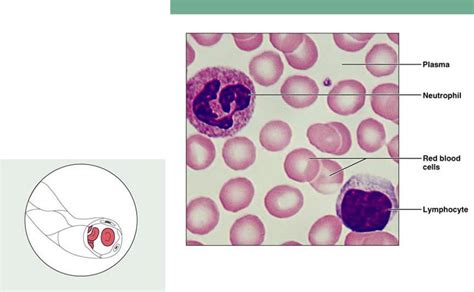
Table of Contents
Red and White Blood Cells in the Fluid Matrix: A Deep Dive into Hematology
The human body is a marvel of engineering, a complex system of interacting components working in perfect harmony. At the heart of this system lies the circulatory system, a network of blood vessels carrying a vital fluid: blood. Blood, far from being a simple liquid, is a complex tissue composed of various cellular components suspended within a fluid matrix, the plasma. This article delves deep into the fascinating world of blood, focusing specifically on the red and white blood cells and their intricate relationship with the plasma, exploring their individual functions, their collaborative efforts, and the implications of imbalances within this dynamic system.
The Fluid Matrix: Plasma – More Than Just a Carrier
Before we delve into the cellular components, let's first appreciate the importance of the fluid matrix, plasma. Plasma isn't just a passive carrier; it's an active participant in maintaining homeostasis. Comprising approximately 55% of blood volume, plasma is a straw-colored liquid consisting primarily of water (around 90%), but it also contains a plethora of essential components:
Key Plasma Components:
-
Proteins: Plasma proteins are vital for maintaining osmotic pressure (albumin), transporting molecules (globulins), and contributing to blood clotting (fibrinogen). The precise protein composition is crucial for blood's viscosity and functionality. Variations can indicate underlying health issues.
-
Electrolytes: Electrolytes like sodium, potassium, calcium, and chloride are crucial for maintaining fluid balance, nerve impulse transmission, and muscle contraction. Their precise concentration is tightly regulated.
-
Nutrients: Plasma carries absorbed nutrients, such as glucose, amino acids, and lipids, from the digestive system to the rest of the body. These nutrients fuel cellular activities and maintain metabolic processes.
-
Hormones: Endocrine glands secrete hormones directly into the bloodstream. Plasma acts as the transport medium, carrying these hormones to their target tissues and organs, coordinating bodily functions.
-
Waste Products: Plasma carries metabolic waste products, such as urea and creatinine, from the tissues to the kidneys for excretion. Efficient removal of these byproducts is critical for preventing toxicity.
-
Gases: Plasma transports oxygen and carbon dioxide. While oxygen is primarily bound to hemoglobin within red blood cells, a small amount is dissolved in plasma. Carbon dioxide is transported in various forms, including dissolved CO2, bicarbonate ions, and carbamino compounds.
Erythrocytes: The Oxygen Carriers – Red Blood Cells
Red blood cells, or erythrocytes, are the most abundant cells in blood, accounting for roughly 40-45% of its volume (hematocrit). Their primary function is oxygen transport from the lungs to the body's tissues and carbon dioxide transport back to the lungs for exhalation. This crucial task is facilitated by their unique structure and composition:
The Unique Structure of Erythrocytes:
-
Biconcave Shape: The unique biconcave shape of erythrocytes maximizes their surface area to volume ratio, increasing the efficiency of oxygen diffusion.
-
Hemoglobin: These cells are packed with hemoglobin, a protein containing iron that binds oxygen. Each hemoglobin molecule can bind up to four oxygen molecules.
-
Lack of Nucleus and Organelles: Mature red blood cells lack a nucleus and other organelles, maximizing the space available for hemoglobin and increasing oxygen-carrying capacity. This also means they have a limited lifespan (approximately 120 days).
Erythropoiesis: The Production of Red Blood Cells
Erythropoiesis, the process of red blood cell production, occurs primarily in the bone marrow. It's tightly regulated by the hormone erythropoietin, produced by the kidneys in response to low oxygen levels (hypoxia). Nutritional factors like iron, vitamin B12, and folate are essential for healthy erythropoiesis. Deficiencies in these nutrients can lead to anemia.
Leukocytes: The Body's Defenders – White Blood Cells
White blood cells, or leukocytes, are the body's immune system's soldiers, defending against infection and disease. Unlike erythrocytes, leukocytes have nuclei and other organelles. They are far less numerous than red blood cells but play a critical role in maintaining health. There are several types of leukocytes, each with specialized functions:
Types of Leukocytes and Their Functions:
-
Neutrophils: These are the most abundant type of leukocyte, acting as the first responders to bacterial and fungal infections. They engulf and destroy pathogens through phagocytosis.
-
Lymphocytes: These are crucial for adaptive immunity. There are three main types:
- B cells: Produce antibodies that target specific pathogens.
- T cells: Directly attack infected cells or help regulate the immune response.
- Natural killer (NK) cells: Kill infected cells and tumor cells.
-
Monocytes: These are large phagocytic cells that engulf pathogens and cellular debris. They differentiate into macrophages in tissues, playing a vital role in chronic inflammation and immune responses.
-
Eosinophils: These cells are involved in combating parasitic infections and allergic reactions.
-
Basophils: These cells release histamine and other mediators involved in allergic reactions and inflammation.
Leukopoiesis: The Production of White Blood Cells
Leukopoiesis, the production of white blood cells, also occurs in the bone marrow. It's a complex process regulated by various cytokines and growth factors, ensuring that the appropriate numbers and types of leukocytes are produced to meet the body's needs.
The Interplay Between Blood Cells and Plasma: A Dynamic Equilibrium
The red and white blood cells don't exist in isolation within the bloodstream; they interact dynamically with the plasma. This interaction is crucial for their proper function and the overall health of the organism.
Oxygen and Carbon Dioxide Transport:
Plasma's role in transporting dissolved gases complements the hemoglobin-mediated oxygen transport by red blood cells. The bicarbonate buffer system in plasma helps regulate blood pH by buffering changes in carbon dioxide levels.
Nutrient and Waste Exchange:
Plasma provides the medium for transporting nutrients to the blood cells and removing waste products. Red blood cells require nutrients like glucose for energy production, while white blood cells need various factors for their activation and function.
Immune Response Coordination:
Plasma plays a vital role in coordinating the immune response. It carries antibodies produced by B cells, chemokines and cytokines that recruit and activate leukocytes, and complement proteins that enhance the ability of phagocytes to eliminate pathogens.
Hemostasis:
Plasma contains clotting factors that are essential for hemostasis, the process of stopping bleeding. Platelets, although not discussed in detail here, also play a crucial role in this process. The interaction between plasma factors and platelets leads to the formation of a blood clot, preventing excessive blood loss.
Clinical Implications: Blood Disorders
Imbalances in the composition or function of blood cells or plasma can lead to various hematological disorders:
Anemia:
Anemia refers to a reduction in the number of red blood cells or the amount of hemoglobin, leading to reduced oxygen-carrying capacity. This can be caused by nutritional deficiencies (iron-deficiency anemia, vitamin B12 deficiency), bone marrow disorders, or chronic diseases.
Leukemias:
Leukemias are cancers of the blood-forming tissues, resulting in an uncontrolled proliferation of abnormal leukocytes. This can impair the body's ability to fight infection and can lead to organ damage.
Thrombocytopenia:
Thrombocytopenia is a deficiency of platelets, leading to increased bleeding risk.
Coagulation Disorders:
Coagulation disorders result from defects in the blood clotting system, leading to increased bleeding risk (hemophilia) or increased risk of thrombosis (formation of blood clots).
Conclusion: A Complex and Vital System
The relationship between red and white blood cells and the fluid matrix of plasma is a complex and tightly regulated system essential for life. Understanding the individual functions of these components and their intricate interactions is crucial for diagnosing and treating a wide range of hematological disorders. Further research continues to unravel the intricacies of this dynamic system, leading to improved diagnostic tools and therapeutic strategies. The continuing exploration of hematology remains a vital pursuit in the quest for better human health.
Latest Posts
Related Post
Thank you for visiting our website which covers about Red And White Blood Cells In Fluid Matrix . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.